Streamlined workflow model for four million sets of radiology images
Filmless OT Project benefits radiology teams and frontline clinicians with enhanced hardware, software and technology in processing, acquisition, retrieval, usage and storage of digitalised radiology images. Below are the sharings from colleagues of different departments on how the project streamlines their workflow, with an ultimate aim to enhance service quality and patient safety.
1. Radiology Department
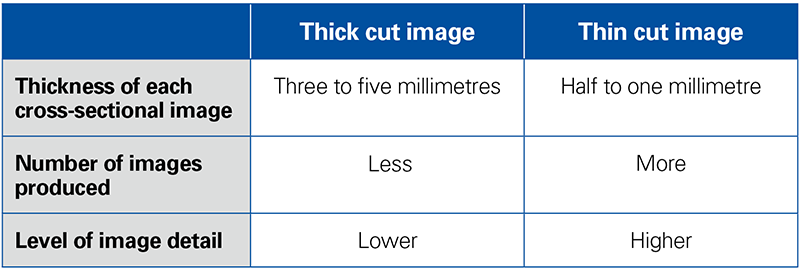
Upload of both ‘thick cut’ and ‘thin cut’ images
Dr Jennifer Khoo, Consultant of Radiology Department from Pamela Youde Nethersole Eastern Hospital, explains how digital radiology images are uploaded to two storage systems after patient’s X-ray, CT or other examinations. One system is used for storing thick cut images, while the other is for thin cut images. Clinicians can enter patient’s HKID number to both systems to view images according to their clinical requirements.
Taking CT brain scan as an example, one examination usually generates about 30 thick cut and 300 thin cut images respectively, among which the latter type provides more details to clinicians.
In the past, transfer of physical imaging films required much manual handling, Dr Khoo continues. “We needed colleagues to select, pack and deliver the physical films to the clinician in person. This practice was time-consuming, labour-intensive and prone to human errors. With the recent enhancement of radiology infrastructure, we have achieved a streamlined, automated workflow which is hassle-free and eliminates the potential risks. Most importantly, it enhances patient safety.”
Thick cut image VS thin cut image
2. Information Technology and Health Informatics Division
Back-end support with an enormous corporate-wide central storage system
Amber Lam, Senior Systems Manager (Clinical Departmental Systems) of Information Technology and Health Informatics Division, says that four million sets of radiology images are produced annually in public hospitals in Hong Kong, among which each set of thin-cut CT constitutes 700 images on the average.
The central storage system in HA data centre serves as a ‘hub’ and has two major functions. It connects to the ‘Picture Archiving Communication System’ of all HA hospitals for uploading and storing radiology images; at the same time, this central storage system is connected to the image processing systems installed inside and outside operating theatres to facilitate and support clinicians’ pre-operative planning. The system keeps a record log with details of data access such as date and time of image access and number of images viewed etc. This record is a safety measure in protecting patients’ privacy and supports future tracking whenever indicated.
3. Image processing systems inside and outside OT
Pre-operative planning shortens operation time
Dr Chan Kwong-shun, Associate Consultant of Department of Surgery, Queen Elizabeth Hospital, is a vascular surgeon who performs operations like endovascular abdominal aortic aneurysm repair and stenting for patients with vascular abnormalities. He frequently uses CT thin cut images for pre-operative planning.
Dr Chan gives an example of how these precise radiology images facilitate his operation planning. Back to the days when there was no CT thin cut image, clinicians could only adjust the position of C-arm X-ray intra-operatively after seeing patient’s anatomical structures. With the assistance of the image processing system, he can now make use of its powerful function like multi-planar reconstruction to conduct assessment and planning before operation, and decide the best approach for the patient. This pre-operative planning allows clinicians to have a thorough understanding of patients’ operative site, and the operation time can therefore be shortened by half to approximately an hour.
In the past, some patients were declined from the operation after considering the operation complexity and risk. As clinicians can now obtain more details through the image processing system and simulate the clinical procedure pre-operatively, the option for operation is now re-opened for some of these marginal cases. Moreover, as these thin cut images can be stored for one year, it supports clinicians to make comparisons on the stent condition during patients’ different phases of rehabilitation.
What is more, the time for clinicians, nurses and supporting staff exposing to X-ray during operations is reduced, which in turn promotes occupational safety and health of clinical staff.
● New technology to enhance patient safety
COVER STORY
● No more boundaries for radiology images
● Development of filmless technology
● Streamlined workflow model for four million sets of radiology images
● Triumph over 9-year uphill struggles
FEATURE
● Restoring the distinct past of KWH
● ‘Like for like’ approach in restoration
PEOPLE
● Young physiotherapist builds a playground in developing country
● Most-loved facilities in the playground
HELEN HA
● Small electrical appliances now available at the online shop
WHAT'S NEW
● New leaders adopt a down-to-earth leadership style
● Mothers’ great companion on the journey of breastfeeding
● Measures to facilitate breastfeeding in workplace
● Make the most out of big data in service planning
● Big data analytics platform to be launched by year-end – no copy and take away of data
STAFF CORNER
● TPH psychiatric rehabilitation centre develops multi-disciplinary training for patients’ recovery
● Fall prevention programme helps elders stay safe and healthy
● 我們都在這裡!(Chinese version only)