Tseung Kwan O Hospital
Enhanced Recovery After Surgery and Patient Blood Management Team
Tseung Kwan O Hospital
Fitter for speedier recovery in operation journey
Patients can win at the starting line when it comes to receiving surgeries. The cross-specialty Tseung Kwan O Hospital Enhanced Recovery After Surgery (ERAS) and Patient Blood Management (PBM) Team revolutionises many dogmas that existed in the pre- and post-operative procedure for treatment, care, recovery and follow up actions by introducing ERAS in November 2015. The programme attempts to optimise patients’ fitness and psychological well-being during the pre-operative period, so that they can expect the ‘big day’ in best conditions. With the respective post-operative care and follow-up administered by the multi-disciplinary team, patients can foresee speedier recovery, a lower chance of complications and a smaller need for blood transfusion.
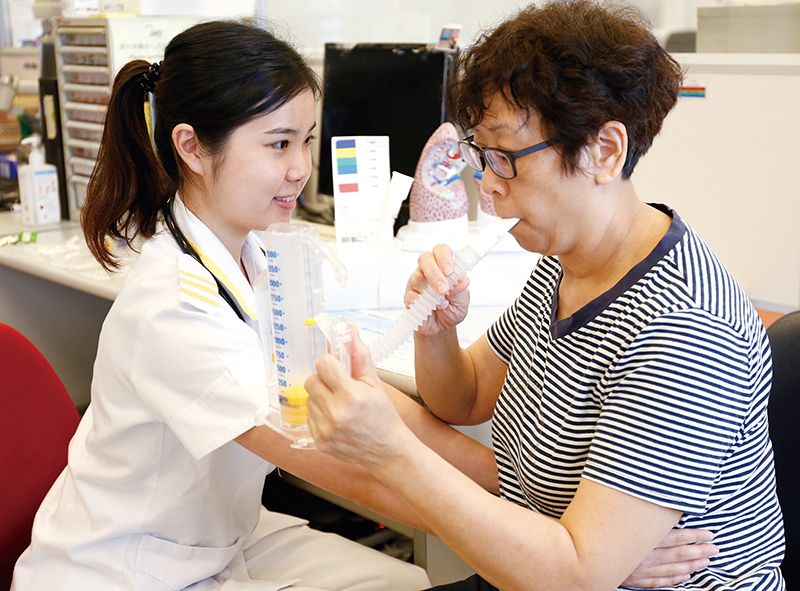
Given that colorectal cancer is the commonest cancer in Hong Kong, the team brought their experience in colorectal cancer surgery. During the, on average, 50-day pre-operative period, patients will meet the surgeon, anaesthesiologist, dietitian, physiotherapist and specialist nurse on the same day for thorough assessment in the Integrated Preoperative Clinic. ‘Prehabilitation’ is the focus in pre-operative stage. Nutritious food is prescribed to patients to manage malnutrition or anaemia. Tammy Fung, Senior Physiotherapist states that physiotherapists will conduct physical fitness and cardiopulmonary evaluations for risk stratification and offer individualised prehabilitation training to patients according to their potential risks of developing post-operative cardiopulmonary complications. Training comprises of aerobic, endurance and resistance exercises utilising treadmills, upper and lower limbs ergometers, steppers, resistance bands and dumbbells to optimise patients’ physical fitness.
One of the team leaders, Dr Kenny Yuen, Chief of Service of Department of Surgery, points out that the multi-disciplinary team members will meet up in wards to conduct a post-operation combined ward round which allows them to share their professional viewpoints and make management decision jointly. The new programme successfully reduces the chance of surgery cancellation due to poor physical conditions of patients. Moreover, thanks to the advances in anaesthesia and surgical skills, patients need not to go through nasogastric tube insertion and prolonged fasting and thus experience less physical and psychological stress. This makes them more ready for minimally invasive surgery. Advanced Practise Nurse Lai Po-lam adds that some patients may doubt if they are ready to get up and walk on the very next day, or even take a few sips of water or milk in the evening of the surgery day.
The team recollects an unforgettable case of a 60-year-old patient with inherited disease who was dependent on breathing machine to sustain life. He was diagnosed to have colorectal cancer and perceived to have high operation risk. After admitting the patient, the team decided to first advise him on prehabilitation strategies before assessing surgery feasibility. Being a high risk patient, he underwent a five-week intensive prehabilitation programme offered by physiotherapists to enhance cardiopulmonary fitness and physical endurance. To avoid worsening his lung functions brought by anaesthesia, the team decided against convention to opt for local anaesthesia and operated on the patient under the monitoring of anaesthesiologist. The surgery was successful. Early mobilisation and intensive chest physiotherapy were commenced the day after surgery under the supervision of physiotherapists on post-operative day two. Amazingly, the patient walked out of the hospital 13 days later.
Another team leader, Dr Cheng Hung-kai, Deputy Hospital Chief Executive and Chief of Service of Department of Anaesthesia & Operating Theatre Services, says that the programme has brought about a paradigm shift in clinical treatment, patient follow-up and medical care. Currently, it is applied to total joint replacement operation, major gynaecological operations (such as hysterectomy) and PBM, with other public hospitals seeking to bring ERAS protocols into practice. He believes, “Not only does the team strive for the same vision, patients’ trust is also our key to success. We will not just stop at this early success and confine ourselves here!”
● Young Achievers pull out all the stops
YOUNG ACHIEVER
● List of young achiever winners
● Small screw makes a big difference in ward
● The compass of healthcare planning
● Passionate scientist develops rapid tests
● Master key man starts occupational safety from staircases
● Fully committed to saving lives from heart
● Nurses light up in patients’ limping road of treatment
● Practical upgrade quality and quantity of PCI service in acute myocardial infarction
● Exercise is key to rehabilitation
● Quick training for new nurses to meet challenges at ease
OUTSTANDING STAFF
● List of outstanding staff winners
● Creative handicrafts help patients restore confidence
● Bring joy to kids during journey against disease
● Pioneer transforms nurse clinic into an integrated sanctuary of care
● Nurturing midwives to ‘walk with women’
● Leader with magnetic personality keeps top team together
OUTSTANDING TEAM
● List of outstanding team winners
● Fulfil the final blessing of life
● HA information at your fingertips
● High-tech simulation enhances task mastery
● A closer look at training equipment
● Replant for a complete body in all endeavours
● Essential tools for replantation surgery
● A dignified end-of-life journey
● Procedures of end-of-life services
● Surgeons go hand-in-hand to enhance surgical efficiency
● Fitter for speedier recovery in operation journey
MERIT LIST
STAFF CORNER