Guide to Trauma Service
|
Trauma Service |
Personnel of Trauma Service (members of TSEC)
Members of Trauma Service Executive Committee (TSEC) as at 2025
| Name | Rank | Department |
|---|---|---|
| Dr Wing Chiu DAI | Consultant – Department of Surgery Director of Trauma Service |
Department of Surgery (Chairman) |
| Dr Theresa LI | CCE | HKWC |
| Dr Tat Chi TSANG | Chief of Service | Department of Accident & Emergency |
| Dr Andy NG | Associate Consultant | Department of Anaesthesia, Pain and Perioperative Medicine |
| Dr Alfred Wong | Consultant | Department of Intensive Care Unit (Adult) |
| Dr Lai Fung LI | Consultant | Department of Neurosurgery |
| Dr Colin YUNG | Associate Consultant | Department of Orthopaedics & Traumatology |
| Dr Kelvin CHOI | Consultant | Department of Radiology |
| Dr Carolette Gronenewald | Associate Consultant | Department of Surgery |
| Ms Celestine NG | Associate Nurse Consultant | Trauma Service (Secretary) |
N.B. Please feel free to contact the TSEC members for suggestions on improvement or quality issues related to Trauma Service.
Primary Trauma Diversion
5 steps Approach:
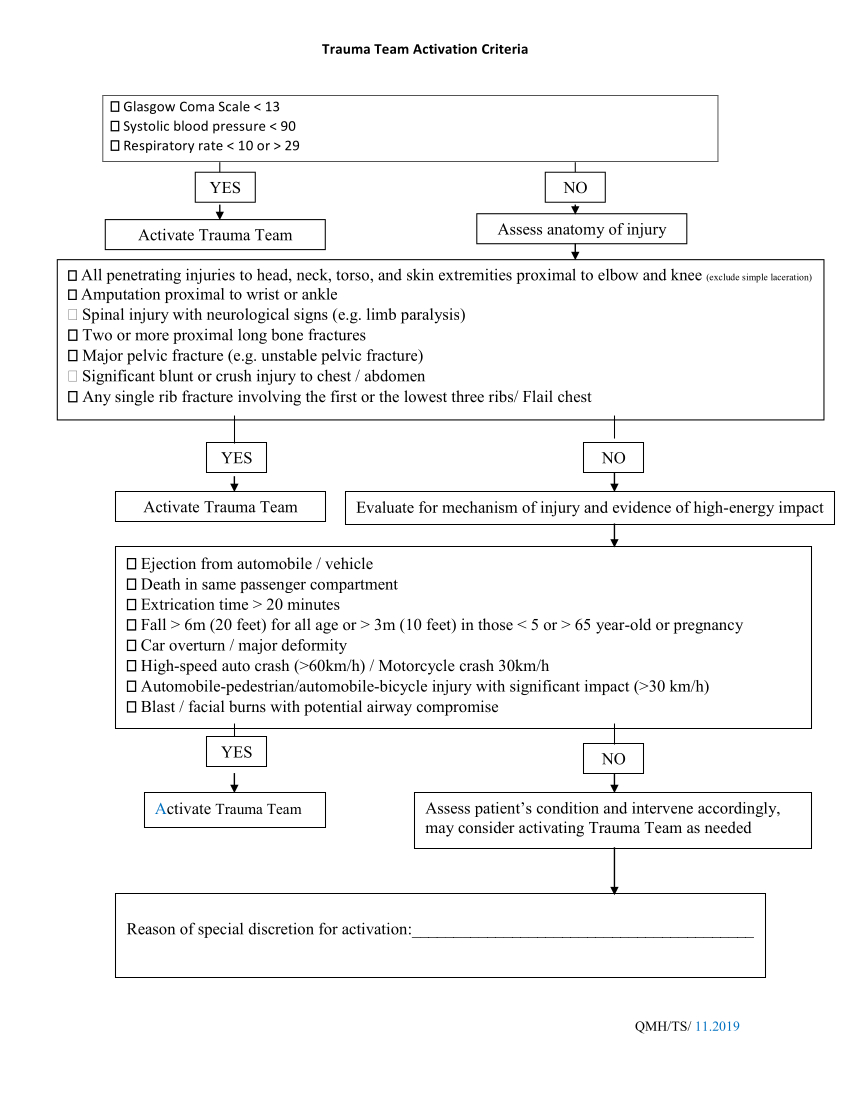
Trauma Team Activation
- Glasgow Coma Scale < 13
- Systolic blood pressure < 90mmHg
- Respiratory rate < 10/min or > 29/min
- All penetrating injuries to head, neck, torso, and skin extremities proximal to elbow and knee (exclude simple laceration)
- Amputation proximal to wrist or ankle
- Spinal injury with neurological signs (e.g. limb paralysis)
- Two or more proximal long bone fractures
- Major pelvic fracture (e.g. unstable pelvic fracture)
- Significant blunt or crush injury to chest / abdomen
- Any single rib fracture involving the first or the lowest three ribs/ Flail chest
- Fall > 6m (20 feet) for all age or > 3m (10 feet) in those < 5 year-old or > 65 year-old or pregnancy
- Fall from 2 times the height of child (age ≤11 year-old)
- Ejection from automobile / vehicle
- Death in same passenger compartment, excluding minibus / bus / coach / train / tram
- Extrication time > 20 minutes
- Car overturn / major deformity
- High-speed auto crash (>60km/h) / Motorcycle crash (>30km/h)
- Automobile-pedestrian/automobile-bicycle injury with significant impact (>30 km/h)
- Blast / facial burns with potential airway compromise
- Gunshot injury
Yes >>Activate Traumatic Brain Injury
No >>Assess patient's condition and intervene accordingly, may consider activating Trauma Team as needed
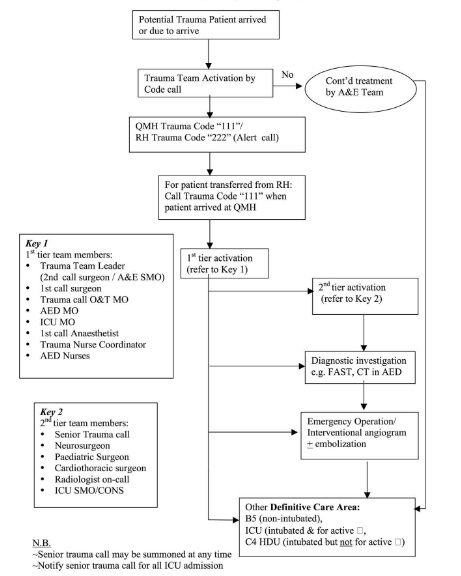
Trauma Team Response System
Calling System for Major Trauma
| Call System | Calling Code | Types of Patients | Members involved | Admission |
|---|---|---|---|---|
| Trauma call for major trauma patient |
|
Major trauma patient who fits the trauma team activation criteria;refer to "Trauma Team Activation Decision Scheme" |
First Tier Members:
On call MOs from different specialties |
|
|
TBI Call (Traumatic Brain Injury) |
|
Patient with severe head injury who fits the trauma team activation criteria but without multiple injuries |
First Tier Members:
Team members from trauma call in case of activating trauma call "111" |
Team Members:Key Roles and Responsibilities
Roles and Responsibilities of Trauma Team Members
Policy:- Team members are responsible for the roles described in the following table.
- Mutual respect, understanding and cooperation must be observed by all.
- The ultimate responsibility rests with the trauma team leader.
| Role | Responsibilities | Who can fill | Mandatory Qualifications |
|---|---|---|---|
| Senior Trauma Call |
|
As delegated by the Department of Surgery |
ATLS certified DSTC certified (desirable) |
| Trauma Team Leader (TTL) |
|
2nd call surgeon/ A&E AC if the former is not present | ATLS certified |
| A&E Doctor 1 |
|
AC A&E or A&E MO i/c | ATLS certified |
| A&E Doctor 2 |
|
MO A&E | |
| Surgery MO |
|
MO 1st call | ATLS certified (desirable) |
| O&T MO |
|
MO 1st call | ATLS certified (desirable) |
| O&T MO |
|
MO 2nd call | ATLS certified (desirable) |
| Anaesthetist or ICU doctor |
|
Anaes. on call/ ICU MO | ATLS certified (desirable) |
| Nursing leader (NL) |
|
Trauma Nurse Coordinator/ Senior Nurse | TNCC/ ATCN certified (desirable) |
| Nurse A |
|
RN/EN | |
| Nurse B |
|
RN/EN | |
| Nurse C |
|
RN/EN |
Radiology Service
X-ray taking in the resuscitation room
- Alert the duty radiographer through the public address system or by phone to come immediately to the resuscitation room.
- Move the X-ray tube to the highest possible level in between shots. Return the tube to parking position immediately after each full examination.
- Resuscitation should continue during X-ray taking. Hence, trauma Team members are encouraged to put on lead aprons for protection, and have the protective side facing the X-ray tube during X-ray taking.
- Comments by radiologists could be obtained on consultation.
- Early notification of trauma case is required before/during meal breaks.
Emergency Ultrasonography
- Urgent ultrasonography is required to detect free fluids in emergency situations by the Trauma Team. It could reduce or avoid unnecessary diagnostic peritoneal lavage in trauma patients.
- During office hours, the radiologist on duty at K3 ultrasound (Ext. 4320) would be called upon to perform emergency ultrasonography for trauma patients in the Resuscitation Room.
- Outside office hours, alert the radiographer on duty at the CT suite (Ext. 4643 or thro??Ext. 3005). The on-call radiologist would be called upon when indicated.
Emergency CT Scan Service
- All trauma call emergency CT will be performed at AED CT on the ground floor of
J block. From 9:00 - 23:00, contact AED CT on-duty radiographer (Dect phone 1579).
From 23:00 - 9:00, contact AED on-call radiographer (Ext 3005). - Trauma Team doctor should accompany the patient during CT scan, be responsible for patient monitoring, and to obtain first hand CT findings.
- The on-call/on-duty radiologist should be notified for IV contrast injection. The Trauma Team Leader may give IV contrast according to the DDR guidelines if the radiologist does not respond within 5 minutes of being called.
- Comments on urgent CT scan performed outside office hours may be requested through the radiographer on duty.
Emergency Angiogram
- During office hours, contact on-duty radiologist at angiogram room (Ext. 4615) for arrangement.
- Outside office hours, contact on-call radiologist at CT suite (Ext. 4643) for arrangement.
NB
- Inform the radiographer i/c for any cancellation.
- Refer to the QMH ?anual for Clinical and Ward Staff??for details.
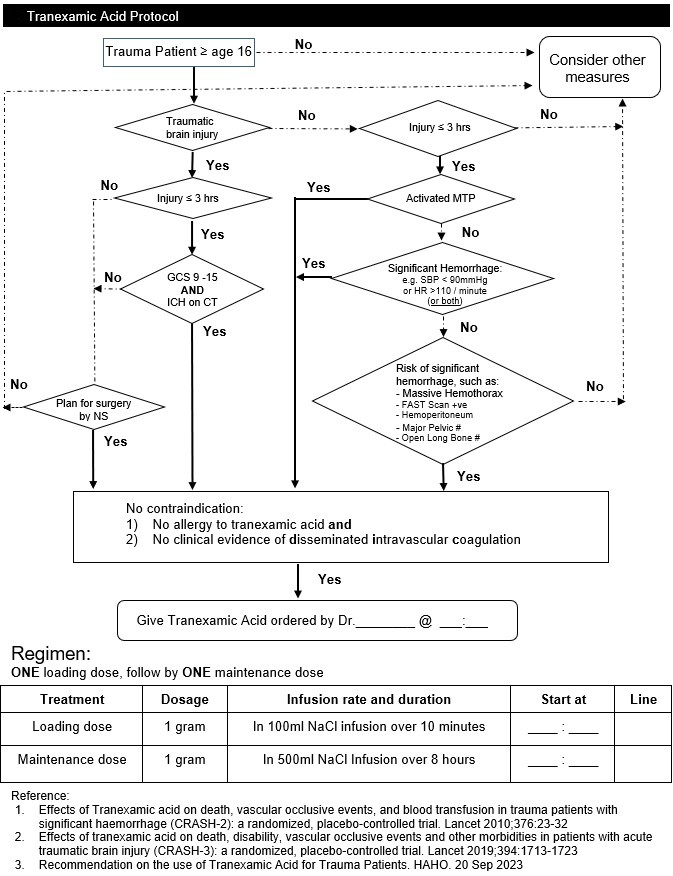
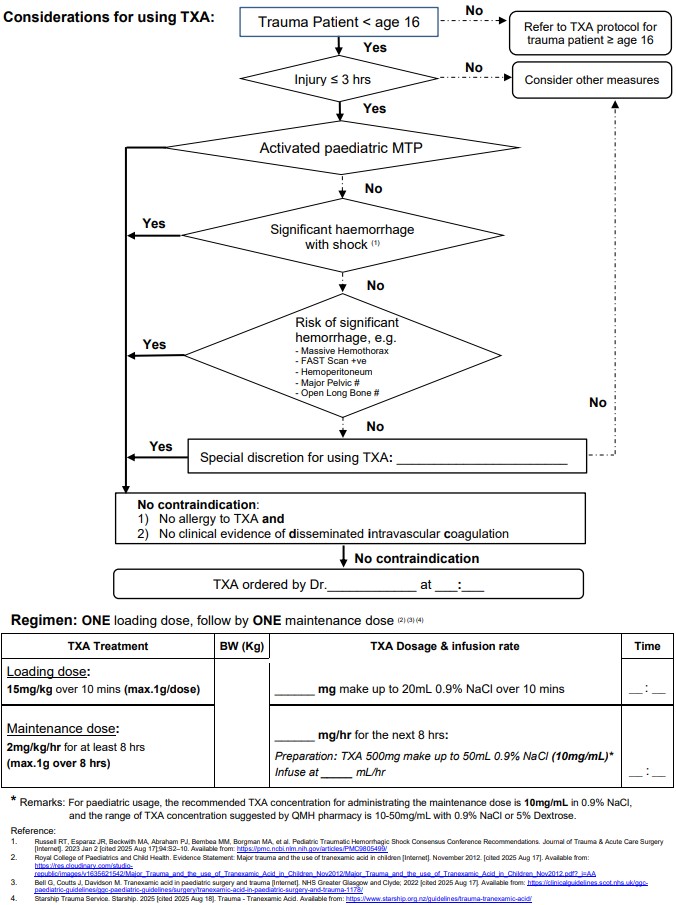
Tranexamic Acid for major trauma patient
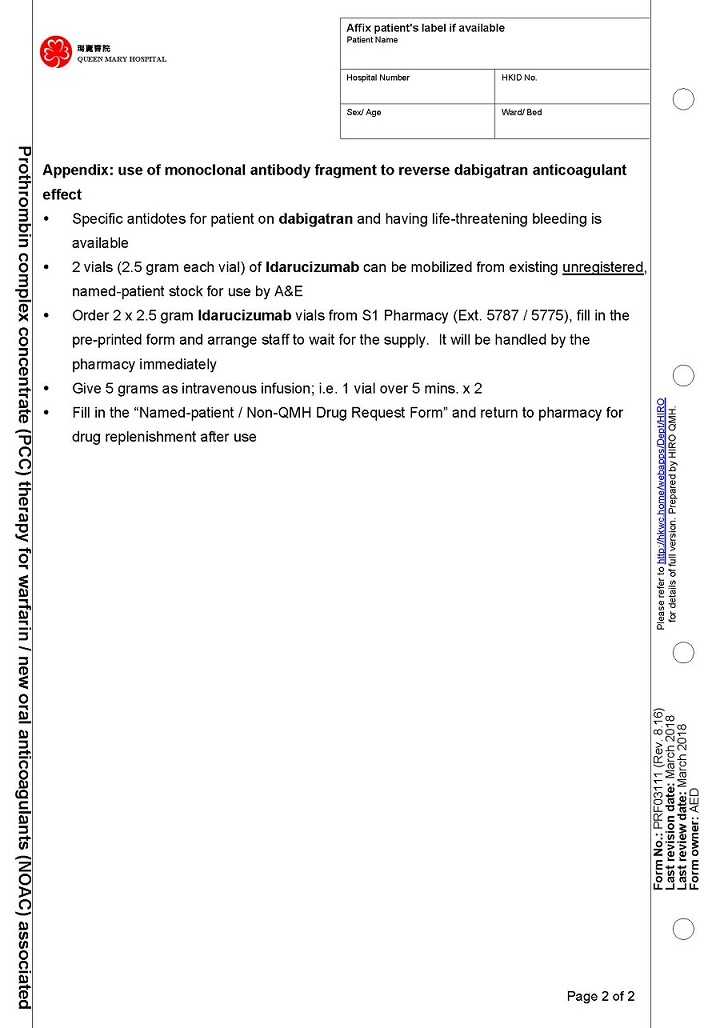
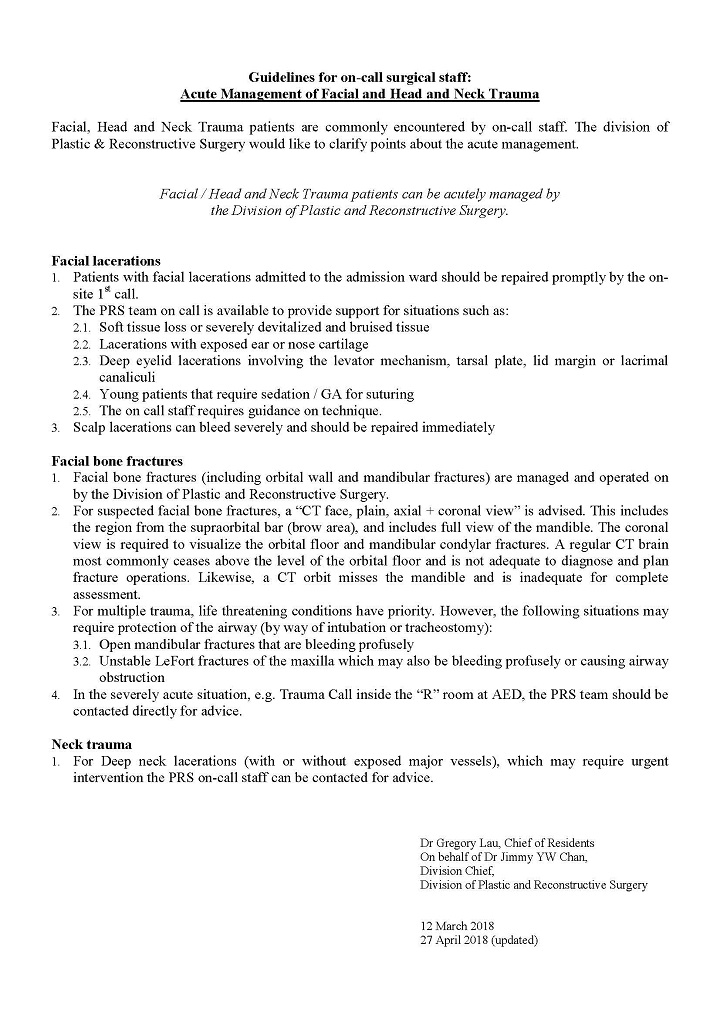
Facial, H&N Trauma
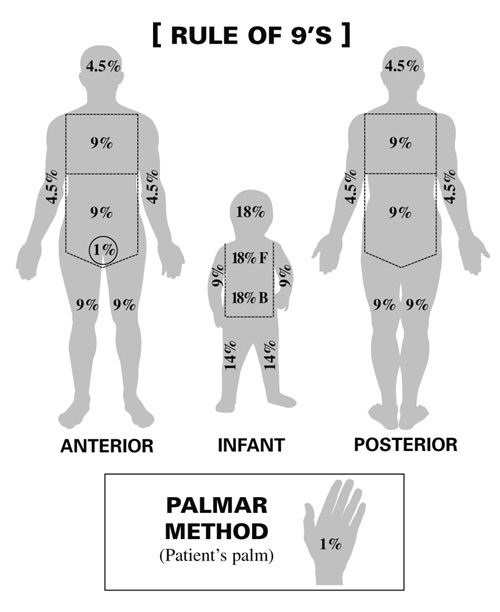
Fluid Resuscitation to Burn
1st 24 hours total fluid = 2-4ml/kg/% of total body surface area (BSA) burned| 24-hour Burn Fluid Calculation example |
|---|
|
|
References
1. ATLS 7th Ed
Drugs used in RSI
A) Induction Agents
- Propofol
o Induction doses of 1.5 to 3 mg/kg IV can be used, titrate to response with a time to effect of approximately 15 to 45 seconds, and a duration of action of 5 to 10 minutes.
o In addition to its use for rapid-sequence induction, propofol is used for sedation for transfer and in critically ill patients.
o Propofol suppresses sympathetic activity, causing myocardial depression and peripheral vasodilation. Reduced dose should be given to patients with underlying hemodynamic instability, as severe hypotension may occur.
- Preparation
o Propofol 10 mg/ml in 20ml ampoule, drawn neat into a 20ml syringe
o Draw another 2 ampoules of propofol into a 50ml syringe (total 40ml of propofol), connected to extension tubing for infusion as sedative agent
|
Drug |
Dosage |
|
Propofol |
1.5 – 3 mg/kg |
|
Propofol infusion |
Starts at 5 – 10 ml/hr and titrate to response |
B) Muscle Relaxants
-
Should only be used by those trained in airway management
-
Suxamethonium is contraindicated in hyperkalaemia, chronic muscle wasting, paraplegia, recent burns. It may also cause a transient rise in intracranial pressure and intraocular pressure
-
Rocuronium is an alternative that can be used when there are contraindications to suxamethonium
- Preparation
o Suxamethonium 50 microgram/ml in a 2ml ampoule, drawn neat into a 3ml syringe
o 2 vials of Rocuronium 10 mg/ml in a 5ml ampoule, drawn neat into a 10ml syringe
|
Drug |
Dosage |
Onset time |
|
Suxamethonium |
1.5 – 2 mg/kg |
30 seconds |
|
Rocuronium |
1.2 mg/kg |
1 minute |
C) Inotropes and vasopressors
- Stand-by inotropes/ vasopressors should be prepared before induction, as there may be significant drop in BP and cardiac output after induction drugs are administered
- Preparation
o Phenylephrine 100 microgram/ml pre-diluted drawn up in a 10ml syringe
o Ephedrine 30 mg/ml added to 4ml of normal saline and drawn into a 5ml syringe, with the final concentration of 6mg/ml
o Atropine 0.6 mg/ml drawn neat into a 3ml syringe
|
Drug |
Dosage |
|
Phenylephrine |
100 microgram boluses, titrated to BP |
|
Ephedrine |
3-6 mg boluses, titrated to BP |
|
Atropine |
10-20 microgram/kg for bradycardia |
D) Other drugs which may be used for induction of anaesthesia
|
Drugs |
Dosage |
Note |
|
Etomidate |
0.2-0.4 mg/kg |
More cardiovascular stable with less drop in BP compared to propofol; however, it causes adrenocortical suppression, inhibiting cortisol and aldosterone synthesis |
|
Thiopentone |
3-7 mg/kg |
Powder form requiring reconstruction with 20ml water to produce 2.5% solution; may precipitate porphyria |
|
Ketamine |
1-2 mg/kg |
Dissociative anaesthesia with analgesic effect, direct stimulation of sympathetic nervous system with increased heart rate/ contractility; may precipitate delirium and hallucinations |
|
Midazolam |
0.1-0.2 mg/kg |
More cardiovascular stable with less drop in BP compared to propofol |
|
Fentanyl |
1-2 microgram/kg |
Blunt cardiovascular response to laryngoscopy |
|
Remifentanil |
0.5-1 microgram/kg |
Ultra-fast and short-acting; blunt cardiovascular response to laryngoscopy, often use as an infusion |
* The above drugs may be selected by those trained and familiar with their use
References:
-
Sympathetic and hemodynamic effects of moderate and deep sedation with propofol in humans. Ebert TJ. Anesthesiology. 2005;103(1):20
-
Gropper, M. A., & Miller, R. D. (2020). Miller’s anesthesia (9th ed.). Elsevier.
-
ACLS Algorithms. American Heart Association. 2020
Analgesics for trauma patients in A&E
Introduction
-
The majority of the major trauma patients experience siginificant pain. Analgesia should not be neglected in trauma patients.
-
Acute pain can be very distressing, and it can lead to complications including hypoventilation, impaired immune response, increased metabolic demand and worsened patient outcome. Effective management of pain in a timely manner is therefore essential.
-
Assessment of pain is critical for providing optimal pain management interventions and it should be done before any painful interventions.
-
Please consult relevant specialists for those in extremes of age (<2 or >70 yr), burns and obstetric patients.
Principle of pain management in traume patients include
-
Early initiation of appropriate treatment
-
Aggressive use of the multimodal therapy
-
Treatment of the underlying cause
-
Assessment and management of the psychosocial factors that may affect treatment and contribute to development of chronic pain
Assessment
-
Pain assessment should be done after primary survey, with frequent reassessments as pain intensity may change over time
-
IV analgesia should be considered for major trauma patients
-
Please refer to separate guideline on pain assessment for trauma patients in A&E
Choice of Analgesics or pain relief
-
Morphine
-
Morphine is a strong opioid which provides effective analgesia for severe trauma pain
-
It is the gold standard for pain relief in trauma and it should be considered as first-line analgesia and dose titrated to achieve adequate analgesia
-
Contraindications:
-
Neuro-trauma patients or those with GCS below 13
-
Airway obstruction or respiratory failure
-
Hypotension or those with hemodynamic instability
-
-
Dosage: Small doses of 1 – 2 mg may be given at 5-minute intervals and titrated to patients' pain scores.
-
-
Ketamine
-
A fast-acting N-methyl-d-aspartate (NMDA) antagonist with relative cardiovascular stability and minimal respiratory depression
-
May depress level of consciousness and cause delirium, which may complicate the clinical picture
-
Contraindications:
-
Severe ischaemic heart disease
-
Heart failure
-
Poorly controlled hypertension
-
Raised intracranial pressure
-
-
Dosage: 0.1-0.3 mg/kg IV bolus with or without infusion (0.1–0.2 mg/kg per hr)
-
-
Paracetamol
-
For mild to moderate pain
-
Contraindications: deranged liver function
-
|
Body weight |
Dosage (IV) |
|
≥50 kg |
1 g every 6 hours; maximum daily dose: 4 g/day |
|
<50 kg |
15 mg/kg every 6 hours; maximum daily dose: 60 mg/kg/day |
-
NSAIDs
-
For mild to moderate pain
-
Do not normally have a role in major trauma due to their deleterious effects on coagulation.
-
Contraindications
-
Ongoing blood loss, bleeding tendency or use of anticoagulants
-
Renal impairment
-
Allergy to NSAIDs
-
GI ulcer, Asthma (for non-specific COX inhibitors)
-
-
Ketorolac
-
Non-specific COX inhibitor
-
Dosage: 30 mg IV as a single dose, or 15-30 mg every 6 hours as needed; maximum daily dose: 120 mg
-
-
Parecoxib
-
COX-2 specific inhibitor
-
Dosage: 40 mg IV bolus, followed by 20-40 mg every 6 to 12 hours as needed; maximum daily dose: 80 mg
-
-
-
Other opioids
-
Other opioid analgesics may be selected by those who are familiar with their use
-
Fentanyl
-
More rapid onset and shorter acting compared to morphine
-
Dosage: 10 to 20 micrograms IV bolus every 5 minutes, titrated to response
-
-
Tramadol
-
A weak opioid for treatment of moderate pain
-
Dosage: 50 mg IV every 6 hours
-
-
-
Splinting of broken bones will aid in pain relief
-
Peripheral nerve block
-
May be performed for specific conditions by trained personnel, with full monitoring and under sterile conditions.
-
Femoral or fascia iliaca block for fractures of femur
-
Brachial plexus block for upper limb injuries
-
Intercostal nerve block for rib fractures
-
Monitoring
-
If patients require strong opioids, regular observations such as SpO2, heart rate, non-invasive blood pressure monitoring, neurological status should be carried out regularly.
-
Resuscitation equipment, medications and personnel should be readily available.
-
Immediate transfer of patient to another department should be avoided after giving strong opioids because of the risk of hypotension and respiratory depression. 15 mins of close observation should be carried out before transfers.
Watch out for adverse effects secondary to opiods
-
Respiratory depression
-
Stop further sedative drugs
-
Assess the Airway, Breathing and Circulation, give oxygen if indicated.
-
Consider giving Naloxone 0.1 – 0.2mg IV bolus, repeated boluses may be required
-
A continuous infusion of naloxone may be required if particular high doses of opioids have been given due to its short half life.
-
-
-
Hypotension
-
Require assessing patient’s general condition and volume status
-
Opioids rarely induce a significant hypotension but the reduction in pain after opioids given can unmask the hypovolaemia in trauma patients.
-
Always consider anaphylaxis as one of the differential diagnoses.
-
-
References
-
National Clinical Guideline Centre (UK). Major Trauma: Assessment and Initial Management. London: National Institute for Health and Care Excellence (NICE); 2016 Feb. PMID: 26913320.
-
Fabbri A, Voza A, Riccardi A, Serra S, Iaco F; Study and Research Center of the Italian Society of Emergency Medicine (SIMEU). The Pain Management of Trauma Patients in the Emergency Department. J Clin Med. 2023 May 5;12(9):3289. doi: 10.3390/jcm12093289. PMID: 37176729; PMCID: PMC10179230.
-
Schwenk ES. Nonopioid pharmacotherapy for acute pain in adults. Post TW, ed. UpToDate. Waltham, MA: UpToDate Inc. http://www.uptodate.com. Accessed August 2024
-
European Society for Emergency Medicine. Guidelines for the management of acute pain in emergency situations. 2020 Available at https://www.eusem.org/images/EUSEM_EPI_GUIDELINES_MARCH_2020.pdf. Accessed August 2024
Traumatic Brain Injury
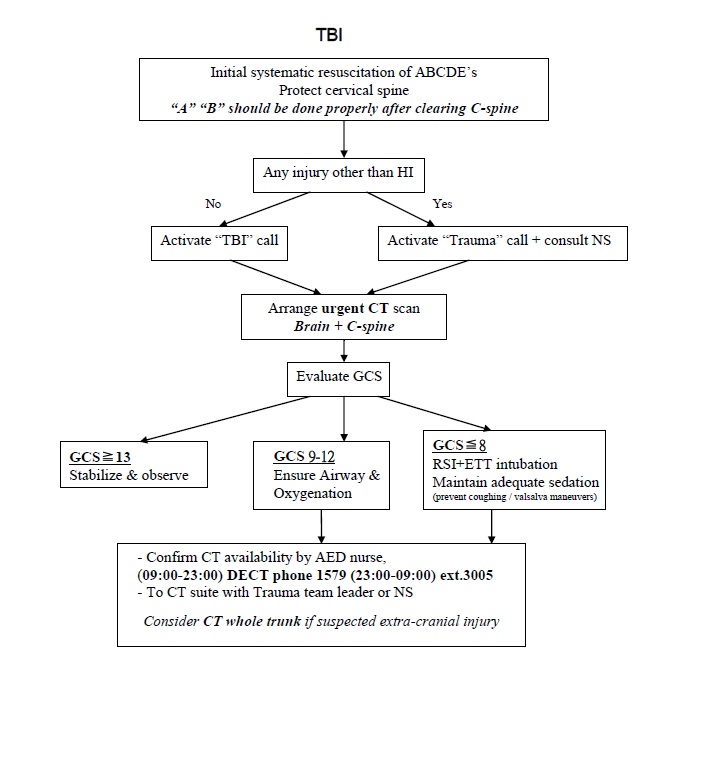 Standard of care for TBI patient
Standard of care for TBI patient
- Head up 30 degree (keep neck collar unless c-spine cleared)
- Maintain normal temperature; prevent / treat hypothermia
- Ventilatory care
- Prolonged prophylactic hyperventilation with partial pressure of carbon dioxide in arterial blood (PaCO2) of 25 mm Hg or less is not recommended
- Keep PaO2 >60mmHg / 8 kPa
- Keep PaCO2 35-40mmg / 4.5-5.5 kPa
- Keep SaO2 >95%
- Blood pressure control
- Maintaining SBP at ??00 mm Hg for patients 50 to 69 years old
- Maintaining SBP at ??10 mm Hg or above for patients 15 to 49 or over 70 years old
- Mannitol 1g/kg (20% 250ml) IV bolus over 30 mins if signs of raise ICP.
- Not if unstable hemodynamics
- Phenytoin (Dilantin) 10mg/kg IV infusion over 1 hour
- Sedation : Midazolam 0.05mg/kg (2-3mg) IV bolus prn for transfer
- Antibiotics:
- Compound vault fracture
- Ceftriaxone (Rocephin) 1gm IV Q12H
- Metronidazole (Flagyl) 500mg IV Q8H
- Skull base fracture with CSF leak
- Augmentin 1.2gm IV Q8H
- Compound vault fracture
- External ventricular drain
- Use of CSF drainage to lower ICP in patients with an initial Glasgow Coma Scale (GCS) <6 during the first 12 hours after injury using an antimicrobial catheter
References:
- Guidelines for the Management of Severe Traumatic Brain Injury 2016. 4th Edition Brain Trauma Foundation
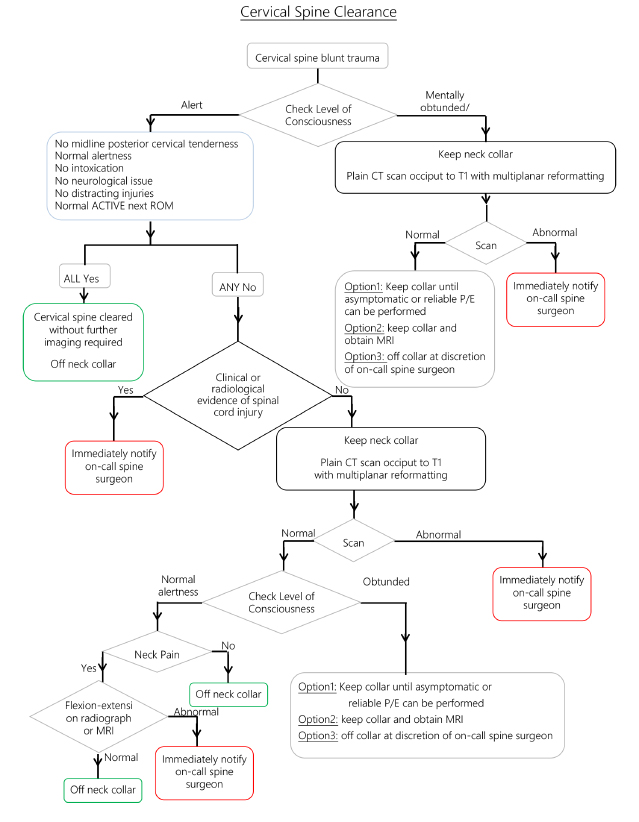
Cervical Spine Clearance
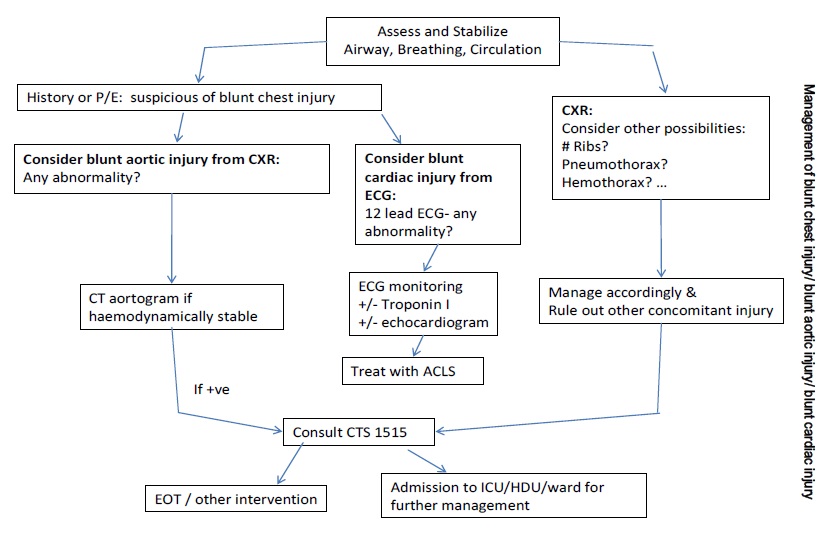
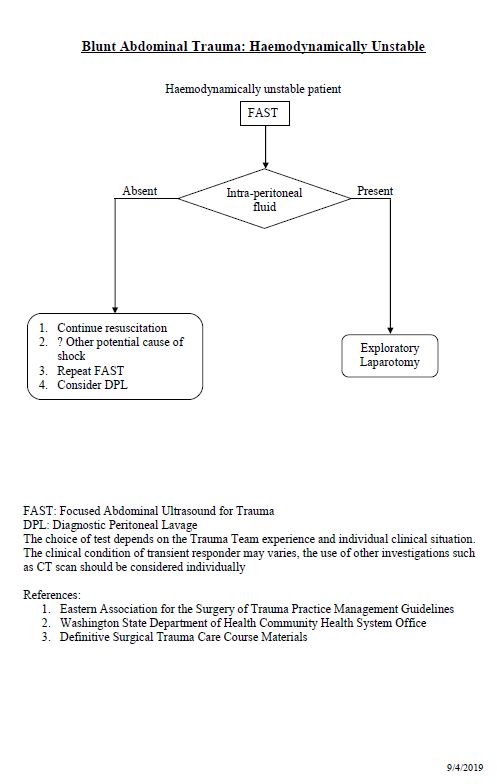
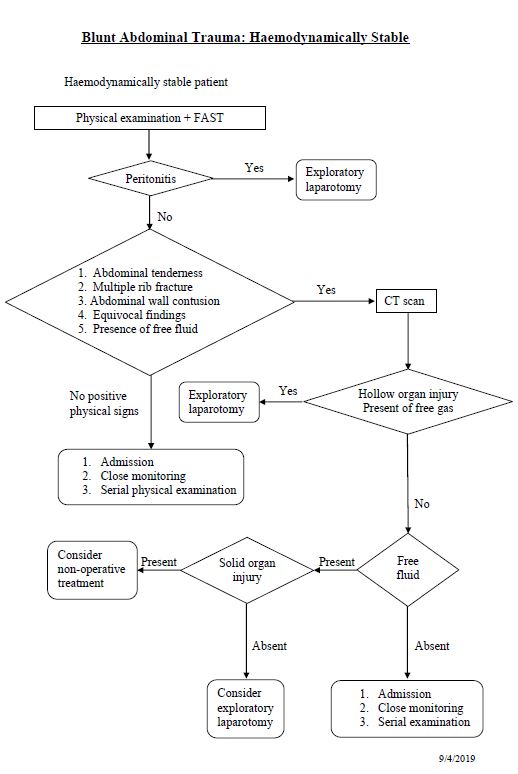
Blunt chest injury/ blunt aortic injury/ blunt cardiac injury
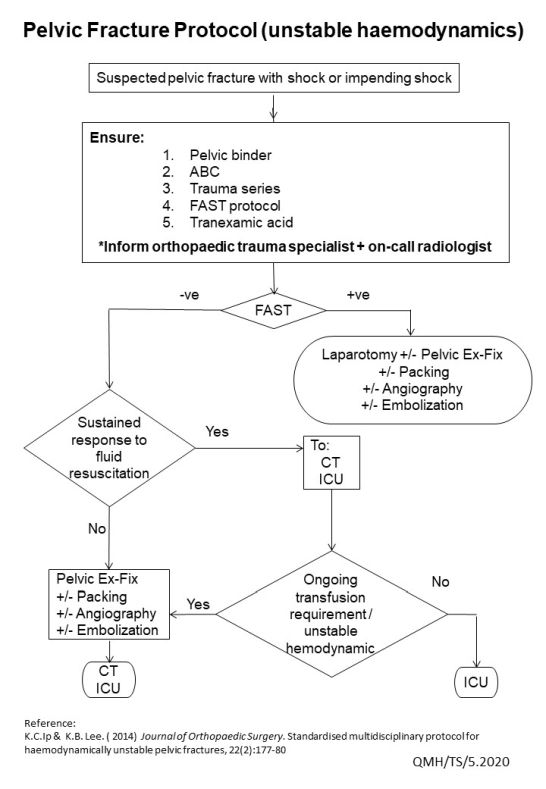
Major Pelvic Trauma
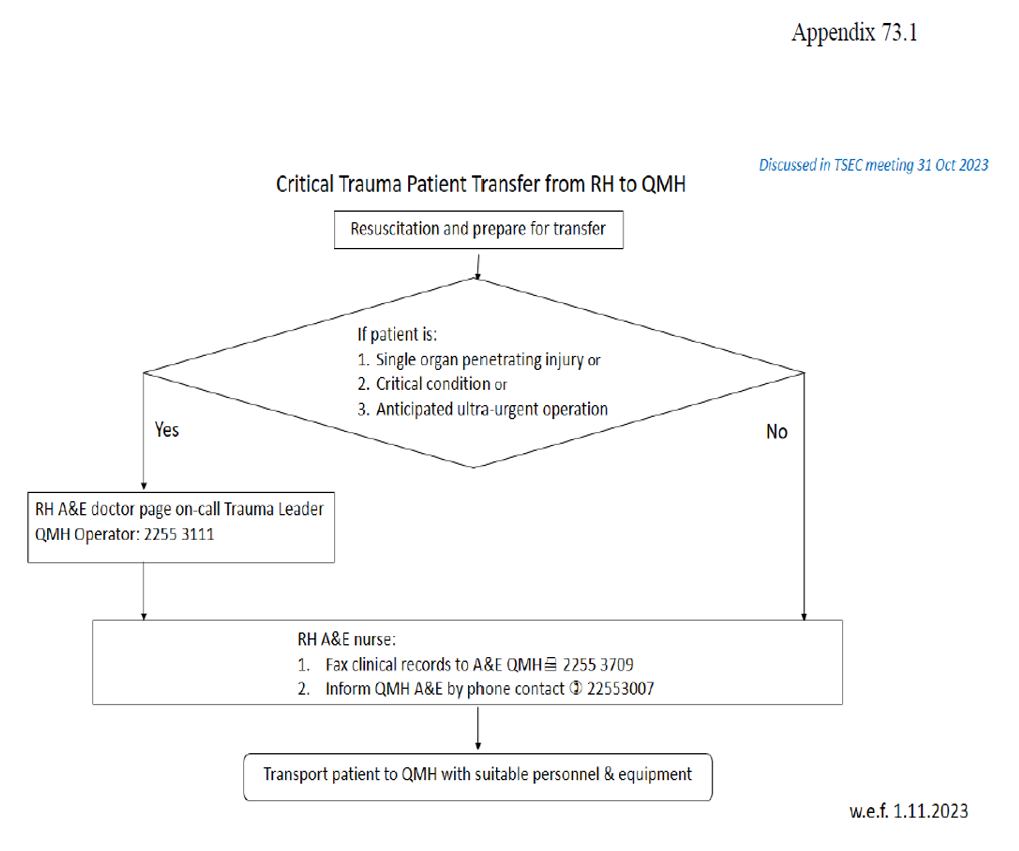
Critical Trauma Patient Transfer from RH to QMH
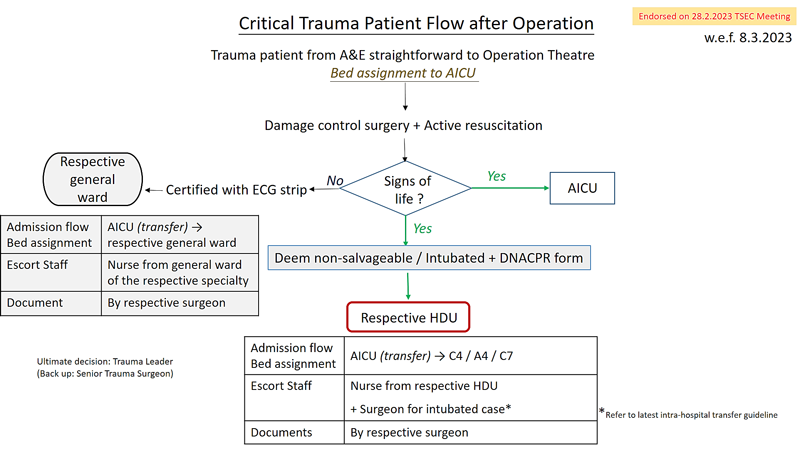
Critical Trauma Patient Flow after Operation
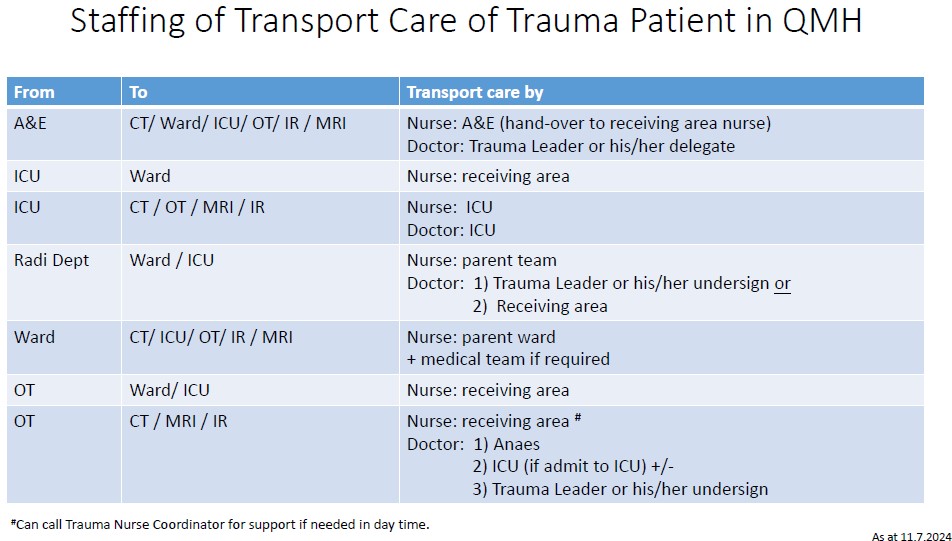
Staffing of Transport Care of Trauma Patient
Adult Glasgow Coma Scale
| Areas of Response | Points |
|---|---|
| Eyes Opening | |
| Eyes open spontaneously | 4 |
| Eyes open in response to voice | 3 |
| Eyes open in response pain | 2 |
| No eye opening response | 1 |
| Best Verbal Response | |
| Oriented (e.g. to person, place, time) | 5 |
| Confused, speaks but is disoriented | 4 |
| Inappropriate, but comprehensible words | 3 |
| Incomprehensible sounds but no words are spoken | 2 |
| None | 1 |
| Best Motor Response | |
| Obeys command to move | 6 |
| Localizes painful stimulus | 5 |
| Withdraws from painful stimulus | 4 |
| Flexion, abnormal decorticate posturing | 3 |
| Extension, abnormal decerebrate posturing | 2 |
| No movement or posturing | 1 |
| Total Possible Points | 15 |
| Major Head Injury | 3 - 8 |
| Moderate Head Injury | 9 -13 |
| Minor Head Injury | 14 -15 |
- The GCS may be falsely low if one of the following is present ??shock, hypoxia, hypothermia, intoxication, post seizure state, sedative drug administration.
- An intubated and pharmacologically paralyzed patient who has GCS of 3 should be recorded as 3 (TP), indicating that the patient was intubated (T) and pharmacologically paralyzed (P).
Vital Signs of Pediatrics for Reference
Vital Signs By Age
| Age | Respiratory Rate/min | Pulse/min | Systolic Blood Pressure(mmHg) |
|---|---|---|---|
| Birth <1 week | 30-60 | 100-160 | 50-70 |
| 1-6 weeks | 30-60 | 100-160 | 70-95 |
| 6 months | 25-40 | 90-120 | 80-100 |
| 1 year | 20-30 | 90-120 | 80-100 |
| 3 years | 25-40 | 90-120 | 80-110 |
| 6 years | 18-25 | 70-110 | 80-110 |
| 10 years | 15-20 | 60-90 | 90-120 |
PEDIATRIC COMA SCALE
Eye Opening
| Score | > 1 Year | < 1 Year |
|---|---|---|
| 4 | Spontaneously | Spontaneously |
| 3 | To verbal command | To shout |
| 2 | No pain | To pain |
| 1 | No response | No response |
Best Motor Response
| Score | > 1 Year | < 1 Year |
|---|---|---|
| 6 | Obeys | Spontaneous |
| 5 | Localizes pain | Localizes pain |
| 4 | Flexion-withdrawal | Flexion-withdrawal |
| 3 |
Flexion-abnormal (decorticate rigidity) |
Flexion-abnormal
(decorticate rigidity) |
| 2 |
Extension (decerebrate rigidity) |
Extension
(decerebrate rigidity) |
| 1 | No response | No response |
Best Verbal Response
| Score | > 5 years | 2 to 5 years | 0 to 23 months |
|---|---|---|---|
| 5 | Oriented and conversess | Appropriate word/phases | Smiles, coos, appropriately |
| 4 | Disoriented and Converses | Inappropriate words | Cries, consolable |
| 3 | Inappropriate words | Persistent crying and screaming | Persistent Inappropriate crying and/or screaming |
| 2 | Incomprehensible sounds | Grunts | Grunts, agitated, restlessness |
| 1 | No response | No response | No response |
Adapted from Simon J. Goldherg A, Prehospital Pediatric Life Suuport, St. Louis, Ma: CV Mosby: 1989:11.
 Trauma Service
Trauma Service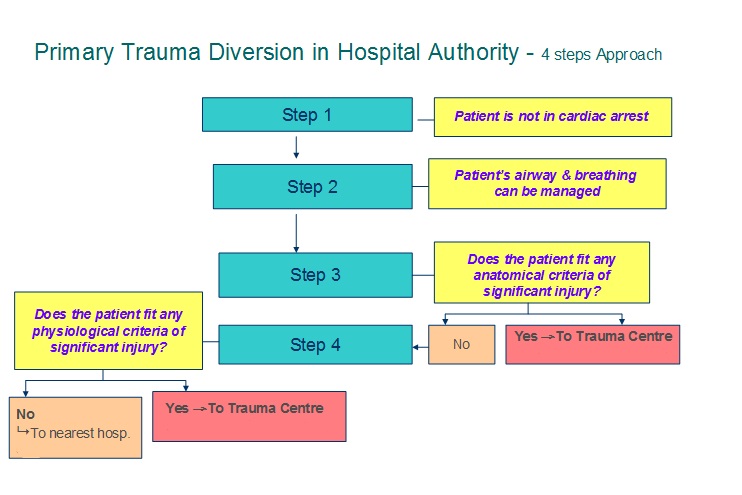
.jpg)
 'Action Button'
'Action Button' 'Add to Home Screen'
'Add to Home Screen' will be added to Home Screen
will be added to Home Screen