United in action
Avian influenza has once again reared its ugly head. As of 17 February, 348 human cases of avian influenza A (H7N9) had been confirmed on the Mainland, while Hong Kong identified its first case in December last year. Public hospitals have implemented a series of preventive measures to better monitor the situation and guard against the spread of the virus. Dr Liu Shao-haei, Chief Manager (Infection, Emergency & Contingency), tells us how staff at Head Office are coordinating with hospitals to fight avian influenza and help people stay healthy.
Prevention is better than cure
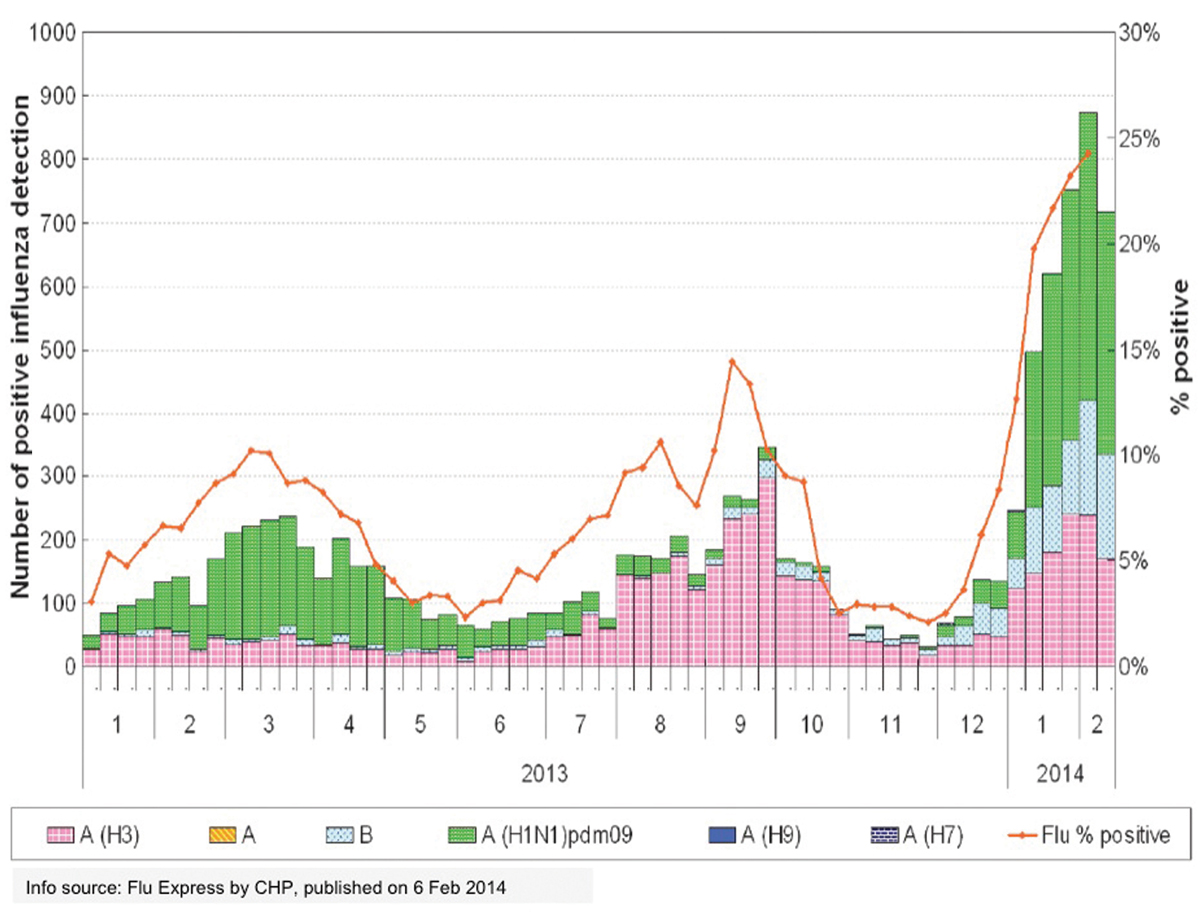
“Hong Kong’s first confirmed case of H7N9 avian influenza A was recorded on 3 December last year. In accordance with the established response mechanism for influenza pandemics, the Hospital Authority worked with the Government to activate the ‘Serious Response Level’ alert, and reminded frontline staff in A&E departments and general outpatient clinics to strengthen surveillance and triage procedures for patients,” Dr Lau says.
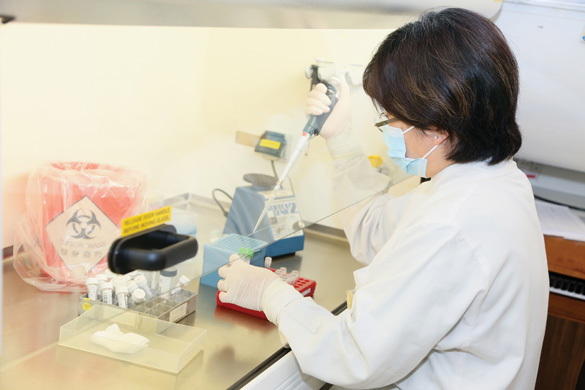
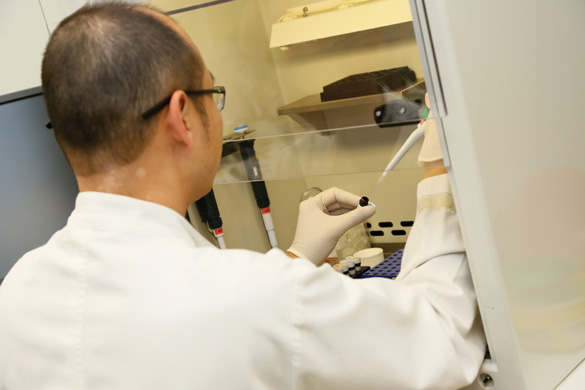
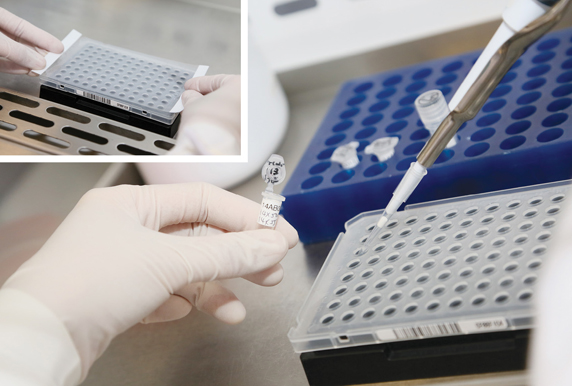
On 6 February this year, HA strengthened the existing surveillance criteria as part of its ‘early reporting, early isolation and early testing’ strategy to minimise the risk of large-scale infection. The Centre for Health Protection will immediately be informed of any patient who is diagnosed as suffering from community-acquired pneumonia and has travelled to an avian flu-affected region within 10 days of becoming ill. Such patients will be placed on an isolation ward and undergo an expedited testing process.
Pre-planning ensures effective response
Dr Liu says: “Preparedness planning has long been an important part of HA’s strategy for controlling the outbreak of contagious diseases.”
In 2006, HA established an Infection, Emergency and Contingency Department at its Head Office with the aim of working to prevent the outbreak of infectious diseases, initiating a rapid response to large-scale disasters and coordinating the management of emergency situations.
The Department is in close and regular contact with HA hospitals, including through the Major Incident Control Centre (MICC), to coordinate response measures with internal and external parties; the Central Committee on Infectious Diseases and Emergency Response, to consolidate input from relevant experts; and the Chief Infection Control Officer Office, to align the standards and practices of hospital infection control teams.
Major Incident Control Centre: key communications hub
The tireless efforts of the entire HA team plays a major role in the Authority’s ability to respond efficiently and effectively to major emergency situations. The MICC plays a pivotal role in emergency situations. In addition to operating as the central monitoring facility, it also serves as the main communication and coordination hub for the HA network.
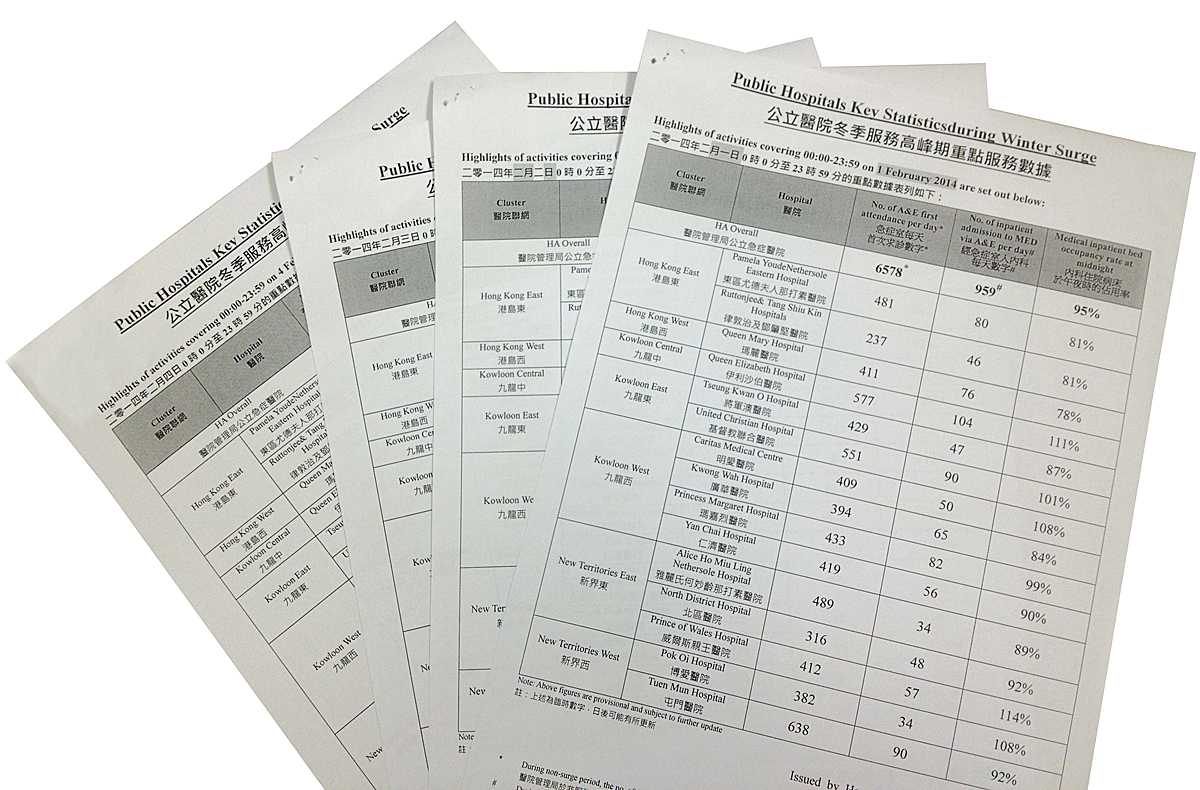
With the recent activation of ‘Serious Response Level’ (S2), the MICC immediately swung into action – communicating closely with Government departments such as the Fire Services Department and the Hong Kong Police Force. At an internal level, it is in close contact with the hospitals – collecting information via the electronic patient record (ePR), Accident and Emergency Information System (AEIS), the electronic influenza surveillance system (eFlu) and the Notifiable Disease Outbreak Reporting System (NDORS). It also disseminates key messages to staff on monitoring and follow-up policies via HA’s rapid communication system.
To help ensure the early isolation of suspected avian influenza cases, the MICC is cooperating with the IT Department to monitor the occupancy rate of isolation wards and help coordinate the efficient use of wards across hospitals.