About Haematopoietic Stem Cell Transplant (HSCT) Service for Paediatrics
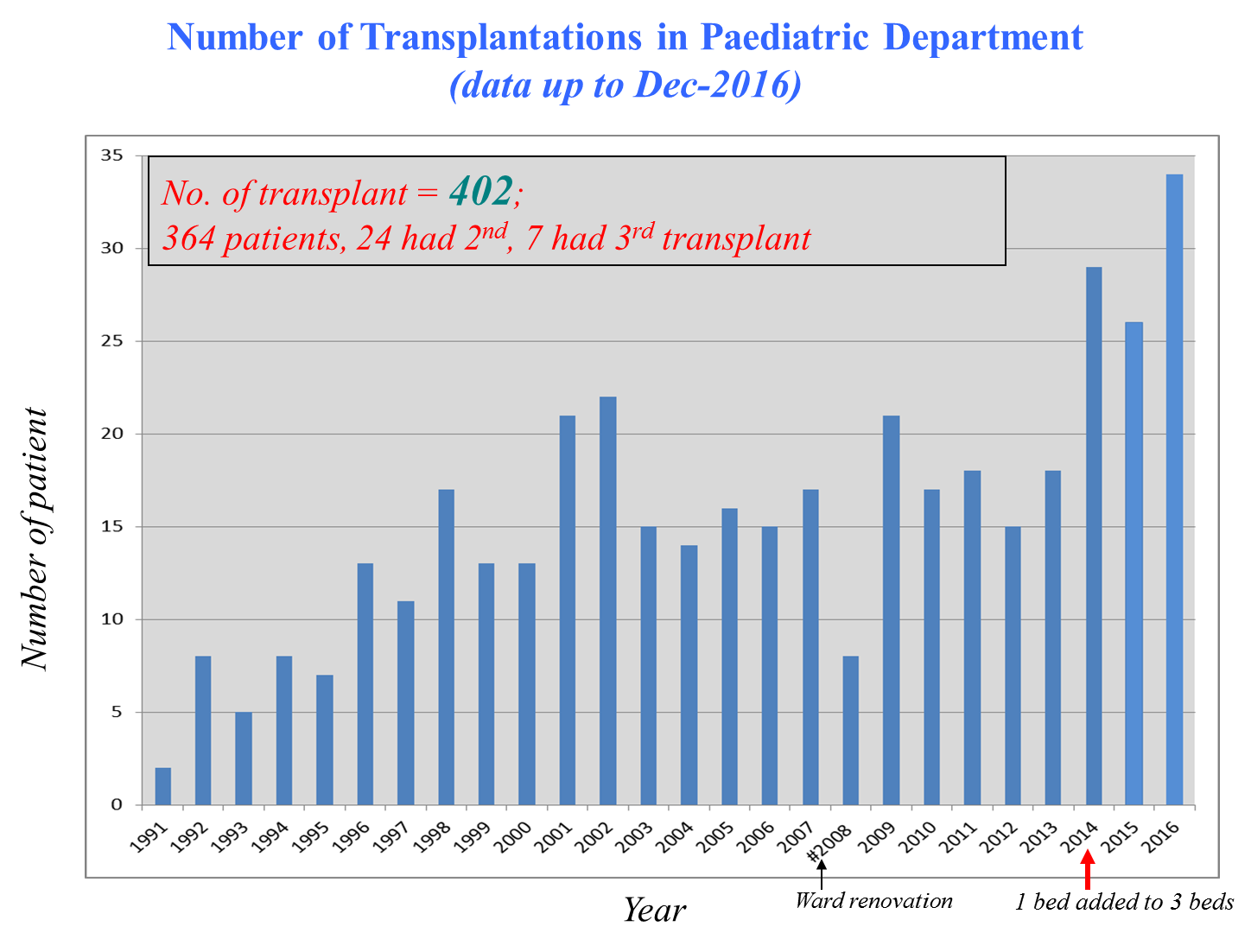
The Children’s Centre for Cancer and Blood Diseases of The Department of Paediatrics and Adolescent Medicine, Queen Mary Hospital has provided haematopoietic stem cell transplant (HSCT) service for children and teenagers since 1991.
Currently, we have 4 HSCT beds in K8N ward, providinga capacity of 30 HSCT procedures per year.
As of December 2016, we have performed 402 HSCT procedures, including 286 allogeneic and 116 autologous HSCT. The spectrum of diseases treated with allogeneic HSCT has expanded rapidly in the past decade, including leukemia, malignant lymphoma, myelodysplastic syndrome, congenital bone marrow failure syndrome such as Fanconi anemia and dyskeratosis congenita, aplastic anemia, transfusion-dependent thalassemia, high-risk solid tumours such as relapsed neuroblastoma, inborn errors of metabolism, and a wide range of primary immunodeficiencies including severe combined immunodeficiency disorder (SCID), Wiskott-Aldrich syndrome, chronic granulomatous disease, leukocyteadhesion deficiency, severe congenital neutropenia, hyper-IgM syndrome, X-linked lymphoproliferative disease, and immune polyendocrinopathy, enteropathy and X-linked (IPEX).Autologous stem cell transplant was performedfor patients with malignant solid tumours following treatment with high dose chemotherapy, and selected patients with autoimmune diseases.
Our center pioneered the use of alternative donor stem cell sources for HSCT,
and was the first in Hong Kong to performed haploidentical stem cell transplant for SCID (1992),
allogeneic (sibling) cord blood transplant for thalassemia major (1994),
unrelated donor HSCT for primary immunodeficiencies (1993) and thalassemia major (2006).
In the recent few years, we have developed protocols for treating relapsed solid tumors using haploidentical family donors, employing state-of-the-art technology such as KIR typing for donor selection, CD3/CD19 depletion,
TCRαβ-CD19 depletion,
CD45RA-depletion or post-transplant cyclophosphamide for depletingalloreactive T-cells. The success rate of HSCT is comparable to international standard.
Donor selection in allogeneic HSCT
The most ideal allogeneic stem cell donor is an HLA-matched sibling. When a patient meets the indication for allogeneic HSCT, his / her siblings will undergo blood test forHLA typing. If an HLA-matched sibling is identified, he / she will undergo donor workup to confirm that he / she is physically suitable for haematopoietic stem cell donation. For paediatric sibling donor, bone marrow harvest is the preferred choice of stem cell collection, and this will be performed under general anaesthesia.
For adult donor, bone marrow or G-CSF mobilized peripheralblood stem cells can be considered.
In some occasions, HLA typing can be done prenatally to determine if the fetus is HLA-matched with the patient;
if matched, cord blood can be collected at the time of delivery and cryopreserved, to be used subsequently for the transplant.
If an HLA-matched sibling is not available, an unrelated donor search will be performed. In children, cord blood transplant is often feasible because of their small size compared with adults. The search for unrelated stem cell donors and cord blood units is coordinated by the Hong Kong Bone Marrow Donor Registry (HKBMDR).
Search will be performed in both local and overseas stem cell registries as well as cord blood banks.
For patients without matched sibling or suitable unrelated donors or cord blood units, mismatched (haploidentical) family donors can be considered as haematopoietic stem cell donors, meaning that there is a good chance that all patients will have a donor,
maximizing the chance of a potential cure of diseases amenable to HSCT.
Milestones of Pediatric HSCT at QMH
The BMT Team, Dept of Paediatrics & Adolescent Medicine
Queen Mary Hospital

NOW
Haploidentical PBSCT (CD45RA depletion)
Disease: ALL
2016
Haploidentical PBSCT (TCRβ depletion)
Disease: Neuroblastoma
2014
Double CBT
Disease: AML
2011
Haploidentical PBSCT (CD3/CD19 depletion)
Disease: MDS-AML
2009
Autologous CBT
Disease: Neuroblastoma
2007
Matched Unrelated BMT
Disease: Thalassaemia Major
2006
Unrelated CBT
Disease: T-ALL
1998
Autologous PBSCT
Disease: Neuroblastoma
Autologous BMT
Disease: Hodgkin Iymphoma
1995
Sibling CBT
Disease: Thal major
1994
Matched unrelated BMT
Disease: WAS
1993
Mismatched related BMT
Disease: SCID
1992
Matched sib BMT (1st case)
Disease: Aplastic anemia
1991
As of December 2016, we have performed 402 HSCT procedures, including 286 allogeneic and 116 autologous HSCT.
 Team Staff
Team Staff
Chief-of-Service and Head
Dr Shau-Yin Ha
Consultant
Dr Alan Kwok-Shing Chiang
Clinical Associate Professor and Honorary Consultant
Dr Daniel Ka-Leung Cheuk
Consultant
Dr Pamela Lee
Clinical Assistant Professor and Honorary Associate Consultant
Ms Connie Wan
Department Operating Manger
Ms Maisie Kan
Ward manager
Ms Scarlett Ho
BMT coordinator
Ms Sau-Ying Chiu
Nurse Specialist
Ms Hau-Yu Chan
Advanced Practice Nurse
 Multi-disciplinary Teams
Multi-disciplinary Teams
Ms Jenny Chan, Mr Chi-On Tsui
Transplantation and Immunogenetics:
Dr Janette Kwok
Radiation Oncology:
Prof Dora Kwong, Dr Patty Ho
Microbiology:
Prof KY Yuen, Dr Pak-Leung Ho
Pathology (haematology section):
Dr Clarence Lam, Dr Rock Leung, Dr Jason So
Clinical Psychology:
Dr Poon Sau Kwan Connie
Children’s Cancer Foundation:
Ms Tammy Loy
Child Life Specialists:
Ms May Lam, Ms Phoebe Ko








