Organ donation: From heartache to serendipity
Organ donation gives new life to those who suffer from organ failure. Immediate identification and referral of donor by frontline colleagues are important, so that patients in need may find a second chance at life.
Once a patient fulfills the following clinical conditions: The Glasgow Coma Scale is under five (G); he has irreversible brain injury (I); he is ventilated (V) and is currently receiving end-of-life care (E), frontline healthcare workers could trigger clinical referral with ‘GIVE’ by referring the potential donor to Organ Donation Coordinator (ODC). When brain death is confirmed, ODC will approach family members of the deceased to seek written consent for donation of deceased organs.
Mabel Chow, ODC of Princess Margaret Hospital, says the traditional value of keeping an intact body was the major barrier to organ donation in the past. “Nowadays most people have an open attitude towards organ donation. However, if the patients did not express their wishes when they were alive, in many cases their family members are not willing to make a decision on behalf.” She understands that the death of a patient comes as a shock and it is not easy for family to make a decision in such a sorrowful time.
Only a brain-dead patient could be a deceased organ donor in Hong Kong, however, the number of patients who could be certified brain death is rather limited. Hence, it is a serendipitous encounter to become an organ donor and recipient. The completion of organ donation and transplant does not refer to a ‘case close’ to the work of an ODC. In general, an ODC would follow up with the donor families all along, which may last for over 10 years for some cases. “I feel so happy that they would see me as their friend. When we accompanied them through a hard time, they would also like to share the happiest moment with us. A donor family even invited us to attend their daughter’s wedding banquet. During the epidemic, one donor family texted me and said they would send me face masks. I was so touched by that. All these motivate me to be an ODC.”
“When all of us are willing to sign-up (register on the Centralised Organ Donation Register), speak-out (your wish to your family and friends), as well as spread-out (the message of organ donation to your family and friends), life can go on. I believe the serendipity develops between the donor and the recipient, would also extend to the ODC, the donor and the recipient families,” says Mabel.
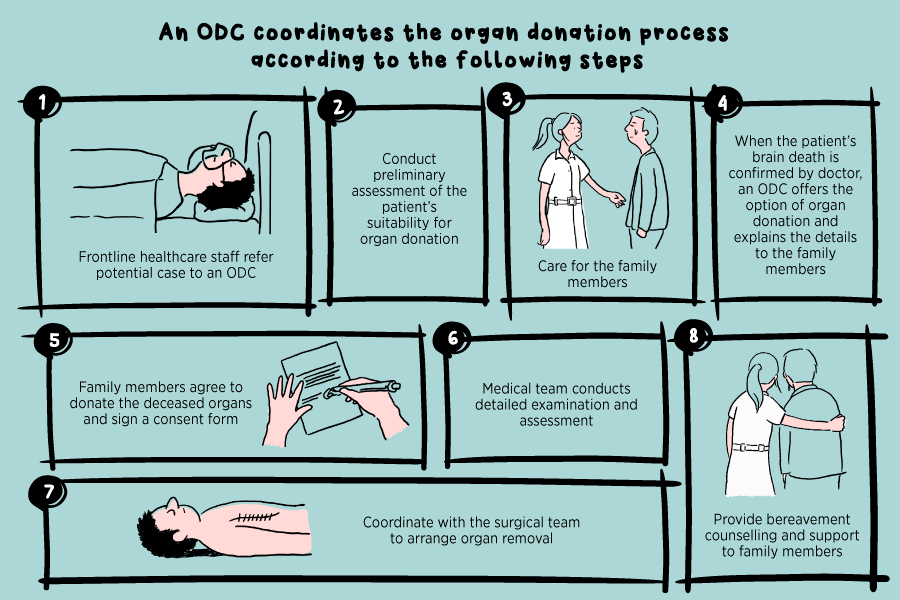
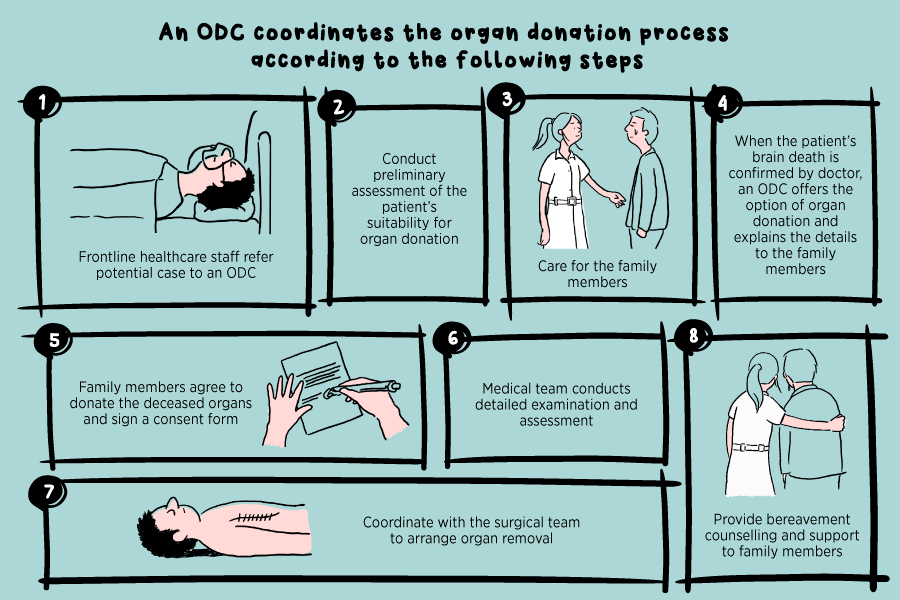
An ODC coordinates the organ donation process according to the following steps:
Once a patient fulfills the following clinical conditions: The Glasgow Coma Scale is under five (G); he has irreversible brain injury (I); he is ventilated (V) and is currently receiving end-of-life care (E), frontline healthcare workers could trigger clinical referral with ‘GIVE’ by referring the potential donor to Organ Donation Coordinator (ODC). When brain death is confirmed, ODC will approach family members of the deceased to seek written consent for donation of deceased organs.
Mabel Chow, ODC of Princess Margaret Hospital, says the traditional value of keeping an intact body was the major barrier to organ donation in the past. “Nowadays most people have an open attitude towards organ donation. However, if the patients did not express their wishes when they were alive, in many cases their family members are not willing to make a decision on behalf.” She understands that the death of a patient comes as a shock and it is not easy for family to make a decision in such a sorrowful time.
Only a brain-dead patient could be a deceased organ donor in Hong Kong, however, the number of patients who could be certified brain death is rather limited. Hence, it is a serendipitous encounter to become an organ donor and recipient. The completion of organ donation and transplant does not refer to a ‘case close’ to the work of an ODC. In general, an ODC would follow up with the donor families all along, which may last for over 10 years for some cases. “I feel so happy that they would see me as their friend. When we accompanied them through a hard time, they would also like to share the happiest moment with us. A donor family even invited us to attend their daughter’s wedding banquet. During the epidemic, one donor family texted me and said they would send me face masks. I was so touched by that. All these motivate me to be an ODC.”
“When all of us are willing to sign-up (register on the Centralised Organ Donation Register), speak-out (your wish to your family and friends), as well as spread-out (the message of organ donation to your family and friends), life can go on. I believe the serendipity develops between the donor and the recipient, would also extend to the ODC, the donor and the recipient families,” says Mabel.
An ODC coordinates the organ donation process according to the following steps:
- Frontline healthcare staff refer potential case to ODC
- Conduct preliminary assessment of the patient's suitability for organ donation
- Care for the family members
- When the patient’s brain death is confirmed by doctor, ODC offers the option of organ donation and explains the details to the family members
- Family members agree to donate the deceased organs and sign a consent form
- Medical team conducts detailed examination and assessment
- Coordinate with the surgical team to arrange organ removal
- Provide bereavement counselling and support to family members