Small changes make a big difference
There are lots of small initiatives for patients inside hospitals. These small changes may seem insignificant, but they are a giant leap that enhances the patients’ experience in seeking medical care and even their quality of life.
 Over 10 years ago when the appointment system was yet introduced, the blood taking room was constantly occupied with people seeking blood taking procedures in the early morning. In this light, the triage system was then adopted to schedule blood taking appointment for patients individually by staff. To enhance efficiency and facilitate patients’ self-care, Queen Mary Hospital had implemented the self-managed bloodtaking scheduling service on a trial basis two years ago, enabling patients to make their appointments with the touch screen kiosks available at different specialist clinics.
Over 10 years ago when the appointment system was yet introduced, the blood taking room was constantly occupied with people seeking blood taking procedures in the early morning. In this light, the triage system was then adopted to schedule blood taking appointment for patients individually by staff. To enhance efficiency and facilitate patients’ self-care, Queen Mary Hospital had implemented the self-managed bloodtaking scheduling service on a trial basis two years ago, enabling patients to make their appointments with the touch screen kiosks available at different specialist clinics.
“It takes only one minute to check the patients’ particulars and another five minutes for the blood taking. However, in the past, a patient could have waited for more than an hour just for this procedure. With the new system in place, patients’ appointments would be evenly allocated among different sessions throughout the day. So now, in most circumstances, the entire procedure only takes around 10 minutes for patients. This also helps avoid gathering of crowds as well as cross-infection amid the COVID-19 epidemic,” says Chan Lai-hung, Cluster General Manager (Nursing), Hong Kong West Cluster, while recalling on her past experience with the overwhelming crowds in the blood taking room.
The hospital sets up the algorithm on the computer, so that the self-managed scheduling system is able to immediately provide patients with several suitable timeslots for blood taking to select based on multiple inputs, such as the next consultation date, the requirement of fasting, the time required according to the respective blood tests, etc. The system is also linked to the mobile application ‘HA Go’, with which users would receive a reminder before the scheduled date for blood taking. Currently these scheduling systems are available in Queen Elizabeth Hospital, United Christian Hospital and Princess Margaret Hospital, and the service is expected to be extended to other hospitals.
 “I have heard some patients with urologic issues grumbling about the struggles they have been facing. Since urinary catheter or urine collection bag has been a necessity for them, they feel more embarrassed than ever to go out, for example, to the restaurant even at their children’s invitation. Their grandchildren also seem hesitant about coming over for a visit. Some patients feel awkward about carrying around the bag in the office. As far as we are concerned about their needs, we have reached out to clothing companies to design these special pants,” says Irene Wu, Ward Manager of Day Surgery Unit of Alice Ho Miu Ling Nethersole Hospital. With an appearance similar to cotton sweatpants, these customised pants are tailored with enlarged pockets such that patients can put the urine collection bags inside.
“I have heard some patients with urologic issues grumbling about the struggles they have been facing. Since urinary catheter or urine collection bag has been a necessity for them, they feel more embarrassed than ever to go out, for example, to the restaurant even at their children’s invitation. Their grandchildren also seem hesitant about coming over for a visit. Some patients feel awkward about carrying around the bag in the office. As far as we are concerned about their needs, we have reached out to clothing companies to design these special pants,” says Irene Wu, Ward Manager of Day Surgery Unit of Alice Ho Miu Ling Nethersole Hospital. With an appearance similar to cotton sweatpants, these customised pants are tailored with enlarged pockets such that patients can put the urine collection bags inside.
This new design is widely welcomed among the patients. As soon as the first 50 pants were given away, another order for 800 pairs of trousers and shorts in black or grey and of different sizes immediately followed. It is estimated that 400 patients will be offered the replenishment, with each getting two of the garments for alternative use. “The patients have had a very pleasant experience with this new design. Their urine collection bags can be easily kept in the pockets without attracting any unwanted attention. Now that they are no longer bothered about always holding the bag as they used to, they can climb stairs safely, live a normal life like most people do and they are no longer trapped at home.”
She hopes that patients from other specialties or with needs of intubation could benefit from this design in the near future. Despite just a slight change to the cutting of pockets, the custom-made design is already a guarantee of a better life quality for the patients.
 In the Ophthalmology Out-patient Clinic at Tung Wah Eastern Hospital (TWEH), you will see a peeping and vibrating tool like one of those you can find in food courts, or simply what we know as the ‘pager system’.
In the Ophthalmology Out-patient Clinic at Tung Wah Eastern Hospital (TWEH), you will see a peeping and vibrating tool like one of those you can find in food courts, or simply what we know as the ‘pager system’.
According to Loretta Siu, Department Operations Manager (Ophthalmology) of TWEH, the common practice in other specialist out-patient clinics is that the patients’ ticket number will be displayed on the screen; whereas this may not be applicable to ophthalmology clinic as the patients concerned suffer from blurry vision and the pillars in the clinic may further block their view. In this regard, a system call may be a solution. “However, we deem this not user-friendly enough for senior ophthalmology patients who also suffer from hearing impairment. Many of our colleagues have the experience that when they call out the patients’ names repeatedly but no one answers. In the meantime, we are aware that such patients are having a hard time with their visual and hearing conditions and keep waiting in the clinic. This has prompted us to step up our efforts and work out a solution for this complex issue.”
Based on medical records or interactions with patients, colleagues at the registration counter would provide patients who suffer from hearing impairment with a wireless tracking device. Nurses at treatment or consultation room would activate the signal transmitter so that the receiver starts blinking and peeping. As such, the patient care assistant is acknowledged to take the patient concerned to the designated room. “Unlike most food courts, our out-patient clinics are located at three separate floor levels. Therefore, we have made requests to the service provider to further amplify the radio frequency,” Loretta adds. The signal can now be detected anywhere in the clinic, which also means the patients seeking consultation are assured to receive the service as needed.
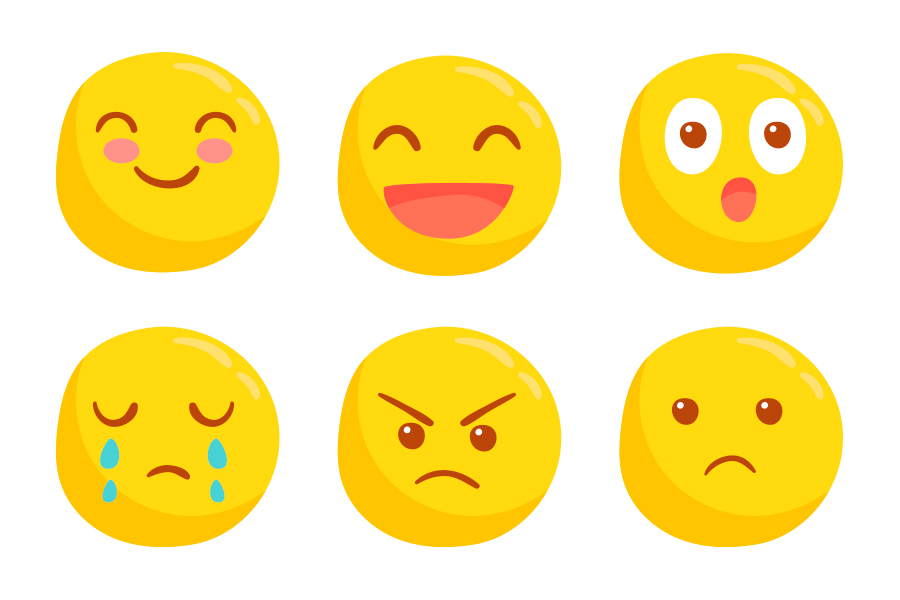 “How do you feel?” For patients with dementia or those relying on end-of-life care, it is undoubtedly difficult for them to express their feelings. In order to help patients with communication disorders to convey emotions, Lai Sin-yee, Clinical Psychologist of Kowloon West Cluster, had built a set of emojis to which patients could point their fingers that match how they feel.
“How do you feel?” For patients with dementia or those relying on end-of-life care, it is undoubtedly difficult for them to express their feelings. In order to help patients with communication disorders to convey emotions, Lai Sin-yee, Clinical Psychologist of Kowloon West Cluster, had built a set of emojis to which patients could point their fingers that match how they feel.
The emojis are a collective representation of the degrees of joy and sadness as well as various emotions such as anger, panic and surprise. Sin-yee explains, “visualised images are useful in clinical communication. The graphics will convey our sincerity to the patients and, through interaction they will explore and understand more clearly how they feel. Using emojis as one kind of mood chart sends important messages to the patient that there are degrees of emotions and that eventually the saddest days will be over. After all, this is to restore hope to the patient.”
When the COVID-19 epidemic was at its worst, the clinical psychology team had arranged video visit in the wards for patients and their family members. “There was an elderly lady who had severe dementia and verbal communication was hardly possible. To facilitate the interaction between the patient and her family members, I guided her to point her fingers to the emojis. Also, we would report the patients’ latest condition to their family members in a brief manner.” Sin-yee adds, using emojis as an ‘ice-breaker’ is effective for the team to ease the patients’ emotions before proceeding to providing relaxation techniques practices or other supports.
More efficient blood taking scheduling
 Over 10 years ago when the appointment system was yet introduced, the blood taking room was constantly occupied with people seeking blood taking procedures in the early morning. In this light, the triage system was then adopted to schedule blood taking appointment for patients individually by staff. To enhance efficiency and facilitate patients’ self-care, Queen Mary Hospital had implemented the self-managed bloodtaking scheduling service on a trial basis two years ago, enabling patients to make their appointments with the touch screen kiosks available at different specialist clinics.
Over 10 years ago when the appointment system was yet introduced, the blood taking room was constantly occupied with people seeking blood taking procedures in the early morning. In this light, the triage system was then adopted to schedule blood taking appointment for patients individually by staff. To enhance efficiency and facilitate patients’ self-care, Queen Mary Hospital had implemented the self-managed bloodtaking scheduling service on a trial basis two years ago, enabling patients to make their appointments with the touch screen kiosks available at different specialist clinics.
“It takes only one minute to check the patients’ particulars and another five minutes for the blood taking. However, in the past, a patient could have waited for more than an hour just for this procedure. With the new system in place, patients’ appointments would be evenly allocated among different sessions throughout the day. So now, in most circumstances, the entire procedure only takes around 10 minutes for patients. This also helps avoid gathering of crowds as well as cross-infection amid the COVID-19 epidemic,” says Chan Lai-hung, Cluster General Manager (Nursing), Hong Kong West Cluster, while recalling on her past experience with the overwhelming crowds in the blood taking room.
The hospital sets up the algorithm on the computer, so that the self-managed scheduling system is able to immediately provide patients with several suitable timeslots for blood taking to select based on multiple inputs, such as the next consultation date, the requirement of fasting, the time required according to the respective blood tests, etc. The system is also linked to the mobile application ‘HA Go’, with which users would receive a reminder before the scheduled date for blood taking. Currently these scheduling systems are available in Queen Elizabeth Hospital, United Christian Hospital and Princess Margaret Hospital, and the service is expected to be extended to other hospitals.
The extraordinary sweatpants
 “I have heard some patients with urologic issues grumbling about the struggles they have been facing. Since urinary catheter or urine collection bag has been a necessity for them, they feel more embarrassed than ever to go out, for example, to the restaurant even at their children’s invitation. Their grandchildren also seem hesitant about coming over for a visit. Some patients feel awkward about carrying around the bag in the office. As far as we are concerned about their needs, we have reached out to clothing companies to design these special pants,” says Irene Wu, Ward Manager of Day Surgery Unit of Alice Ho Miu Ling Nethersole Hospital. With an appearance similar to cotton sweatpants, these customised pants are tailored with enlarged pockets such that patients can put the urine collection bags inside.
“I have heard some patients with urologic issues grumbling about the struggles they have been facing. Since urinary catheter or urine collection bag has been a necessity for them, they feel more embarrassed than ever to go out, for example, to the restaurant even at their children’s invitation. Their grandchildren also seem hesitant about coming over for a visit. Some patients feel awkward about carrying around the bag in the office. As far as we are concerned about their needs, we have reached out to clothing companies to design these special pants,” says Irene Wu, Ward Manager of Day Surgery Unit of Alice Ho Miu Ling Nethersole Hospital. With an appearance similar to cotton sweatpants, these customised pants are tailored with enlarged pockets such that patients can put the urine collection bags inside.
This new design is widely welcomed among the patients. As soon as the first 50 pants were given away, another order for 800 pairs of trousers and shorts in black or grey and of different sizes immediately followed. It is estimated that 400 patients will be offered the replenishment, with each getting two of the garments for alternative use. “The patients have had a very pleasant experience with this new design. Their urine collection bags can be easily kept in the pockets without attracting any unwanted attention. Now that they are no longer bothered about always holding the bag as they used to, they can climb stairs safely, live a normal life like most people do and they are no longer trapped at home.”
She hopes that patients from other specialties or with needs of intubation could benefit from this design in the near future. Despite just a slight change to the cutting of pockets, the custom-made design is already a guarantee of a better life quality for the patients.
Wireless tracking device for hearing impaired patients
 In the Ophthalmology Out-patient Clinic at Tung Wah Eastern Hospital (TWEH), you will see a peeping and vibrating tool like one of those you can find in food courts, or simply what we know as the ‘pager system’.
In the Ophthalmology Out-patient Clinic at Tung Wah Eastern Hospital (TWEH), you will see a peeping and vibrating tool like one of those you can find in food courts, or simply what we know as the ‘pager system’.
According to Loretta Siu, Department Operations Manager (Ophthalmology) of TWEH, the common practice in other specialist out-patient clinics is that the patients’ ticket number will be displayed on the screen; whereas this may not be applicable to ophthalmology clinic as the patients concerned suffer from blurry vision and the pillars in the clinic may further block their view. In this regard, a system call may be a solution. “However, we deem this not user-friendly enough for senior ophthalmology patients who also suffer from hearing impairment. Many of our colleagues have the experience that when they call out the patients’ names repeatedly but no one answers. In the meantime, we are aware that such patients are having a hard time with their visual and hearing conditions and keep waiting in the clinic. This has prompted us to step up our efforts and work out a solution for this complex issue.”
Based on medical records or interactions with patients, colleagues at the registration counter would provide patients who suffer from hearing impairment with a wireless tracking device. Nurses at treatment or consultation room would activate the signal transmitter so that the receiver starts blinking and peeping. As such, the patient care assistant is acknowledged to take the patient concerned to the designated room. “Unlike most food courts, our out-patient clinics are located at three separate floor levels. Therefore, we have made requests to the service provider to further amplify the radio frequency,” Loretta adds. The signal can now be detected anywhere in the clinic, which also means the patients seeking consultation are assured to receive the service as needed.
Emojis as ice-breaker
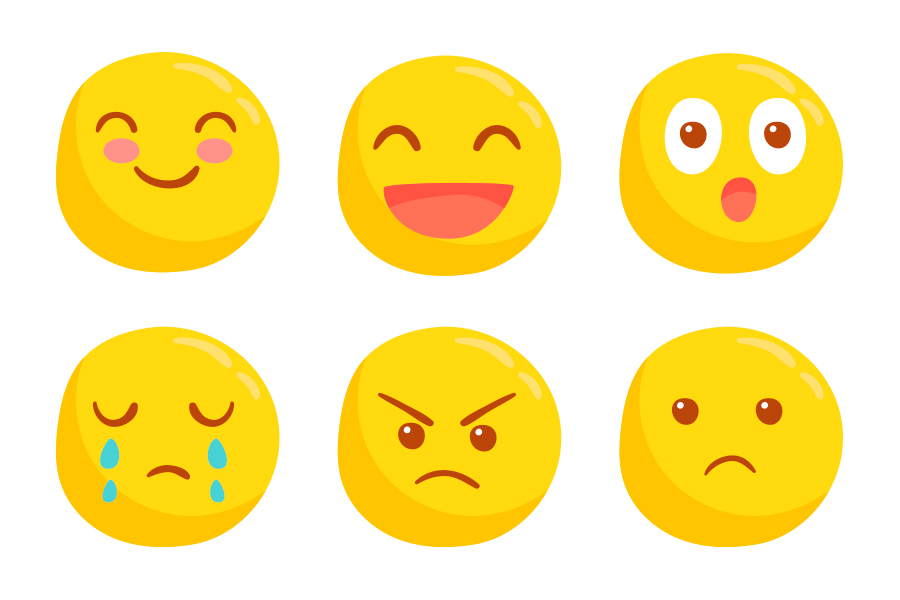 “How do you feel?” For patients with dementia or those relying on end-of-life care, it is undoubtedly difficult for them to express their feelings. In order to help patients with communication disorders to convey emotions, Lai Sin-yee, Clinical Psychologist of Kowloon West Cluster, had built a set of emojis to which patients could point their fingers that match how they feel.
“How do you feel?” For patients with dementia or those relying on end-of-life care, it is undoubtedly difficult for them to express their feelings. In order to help patients with communication disorders to convey emotions, Lai Sin-yee, Clinical Psychologist of Kowloon West Cluster, had built a set of emojis to which patients could point their fingers that match how they feel.
The emojis are a collective representation of the degrees of joy and sadness as well as various emotions such as anger, panic and surprise. Sin-yee explains, “visualised images are useful in clinical communication. The graphics will convey our sincerity to the patients and, through interaction they will explore and understand more clearly how they feel. Using emojis as one kind of mood chart sends important messages to the patient that there are degrees of emotions and that eventually the saddest days will be over. After all, this is to restore hope to the patient.”
When the COVID-19 epidemic was at its worst, the clinical psychology team had arranged video visit in the wards for patients and their family members. “There was an elderly lady who had severe dementia and verbal communication was hardly possible. To facilitate the interaction between the patient and her family members, I guided her to point her fingers to the emojis. Also, we would report the patients’ latest condition to their family members in a brief manner.” Sin-yee adds, using emojis as an ‘ice-breaker’ is effective for the team to ease the patients’ emotions before proceeding to providing relaxation techniques practices or other supports.