Freeing dialysis patients from years of pain

“The stress and obstacles we encountered during the procedure were nowhere near the patients had suffered before the transplant,” says Lee Shuk-hang, Nursing Consultant of Department of Renal Care of PMH, who worked closely with the two donor families to prepare for the operations and monitor the patients afterwards.
For most patients with end-stage renal failure, kidney transplantation is the best treatment option. Currently, there are about 2,000 people on the deceased allocation waitlist in Hong Kong, and the average waiting time for a successful kidney transplant is six years. Patients receive renal replacement therapy when they wait for transplantation. More than 1,700 patients a year receive hemodialysis in public hospitals while more than 4,000 receive peritoneal dialysis.
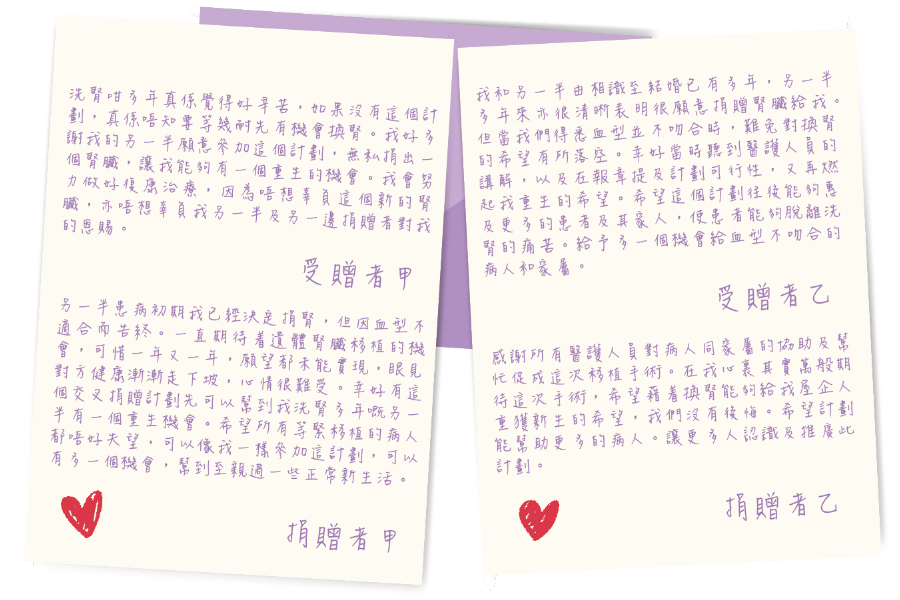
Before the landmark operations, the two patients had been receiving hemodialysis following six to seven years each of peritoneal dialysis. One of the patients was successfully matched with a cadaveric kidney but was unable to go ahead with the operation due to peritonitis. The journey to the operating theatre, therefore, was a long and winding one and it took many matches before everything finally fell into place. “I was impressed by their mental strength,” Ms Lee says. “There were inevitable disappointments in the process, but they never gave up.”
For most patients with end-stage renal failure, kidney transplantation is the best treatment option. Currently, there are about 2,000 people on the deceased allocation waitlist in Hong Kong, and the average waiting time for a successful kidney transplant is six years. Patients receive renal replacement therapy when they wait for transplantation. More than 1,700 patients a year receive hemodialysis in public hospitals while more than 4,000 receive peritoneal dialysis.
Before the landmark operations, the two patients had been receiving hemodialysis following six to seven years each of peritoneal dialysis. One of the patients was successfully matched with a cadaveric kidney but was unable to go ahead with the operation due to peritonitis. The journey to the operating theatre, therefore, was a long and winding one and it took many matches before everything finally fell into place. “I was impressed by their mental strength,” Ms Lee says. “There were inevitable disappointments in the process, but they never gave up.”
Waking up to a bright new reality
The first question and biggest concern that the donor at PMH had after the successful pair kidney transplant was not about the own health but the condition of the family member who received the organ.
That selfless gesture of compassion impressed Dr Samuel Fung, the Chairperson of Paired Kidney Donation Working Group of HA, who helped coordinating the multidisciplinary teams in the final preparation for the patients to ensure they were suitable for the surgery. Dr Fung worked in partnership with Dr Maggie Ma, Co-Director of Combined Renal Replacement Services of QMH, who conducted the examinations of the patients at her hospital.
Even if the matches were found to be successful, there were still many factors that would determine if surgery could go ahead, Dr Ma explains. As well as preparing the operating theatres and surgical teams, there were the challenges of a tight deadline with a series of tests that had to be completed within three months, including renal and urological exams, clinical psychologist evaluations, and COVID-19 vaccinations, while ensuring the patients’ medical conditions were kept under control. “We understood the uncertainty, so we continued to manage the patients' expectations and keep them informed of all possible scenarios,” Dr Ma says. “Needless to say, we are thrilled with the success of this surgery. It lays the groundwork for the next operations of this kind.”
Dr Fung believes the greatest challenge for future operations will be the coordination of resources. “The paired kidney donation (PKD) programme would need staff and operating theatres,” he says. “If PKD becomes more prevalent in the future, more patients and their families will benefit. PKD is definitely a viable option. More potential patients are encouraged to join the matching pool. If they do that, more patients will be freed from the ordeals of receiving hemodialysis and peritoneal dialysis, and they can begin new lives after the operations.”
That selfless gesture of compassion impressed Dr Samuel Fung, the Chairperson of Paired Kidney Donation Working Group of HA, who helped coordinating the multidisciplinary teams in the final preparation for the patients to ensure they were suitable for the surgery. Dr Fung worked in partnership with Dr Maggie Ma, Co-Director of Combined Renal Replacement Services of QMH, who conducted the examinations of the patients at her hospital.
Even if the matches were found to be successful, there were still many factors that would determine if surgery could go ahead, Dr Ma explains. As well as preparing the operating theatres and surgical teams, there were the challenges of a tight deadline with a series of tests that had to be completed within three months, including renal and urological exams, clinical psychologist evaluations, and COVID-19 vaccinations, while ensuring the patients’ medical conditions were kept under control. “We understood the uncertainty, so we continued to manage the patients' expectations and keep them informed of all possible scenarios,” Dr Ma says. “Needless to say, we are thrilled with the success of this surgery. It lays the groundwork for the next operations of this kind.”
Dr Fung believes the greatest challenge for future operations will be the coordination of resources. “The paired kidney donation (PKD) programme would need staff and operating theatres,” he says. “If PKD becomes more prevalent in the future, more patients and their families will benefit. PKD is definitely a viable option. More potential patients are encouraged to join the matching pool. If they do that, more patients will be freed from the ordeals of receiving hemodialysis and peritoneal dialysis, and they can begin new lives after the operations.”