Innovation
New technologies applied in medical settings
Every crisis creates problems, yet lies opportunities also. During the COVID-19 outbreak, colleagues have overcome various challenges in frontline services with creativity and leverage on technology. The following are some outstanding examples.
Self-developed system optimises risk assessment
In view of the clusters of COVID-19 infections in Kowloon Central Cluster (KCC), Information Technology Department of KCC developed and launched the Residential Address Search System in mid-July. Wallace Cheng, System Manager of the Department, explains that the system extracts daily updates on the list of buildings with confirmed cases from the Centre for Health Protection. When authorised medical staff enter a patient’s ID number or scan his barcode, the system will be able to identify whether the patient resides in a high-risk place or building by referring to the registered address. This tool is proven to effectively enhance risk assessment, and hence facilitate arrangements for isolation facilities and provision of testings for patients, which further minimises the risk of transmission.

’DeliverBot’ in isolation wards
Queen Elizabeth Hospital has introduced ‘DeliverBot’ in assisting deliveries of meals, linens and other supplies to patients, so as to reduce colleagues’ direct contact with patients and hence the risks of infection, as well as to save time in donning and doffing personal protective equipment. The robot helper is equipped with three trays and multiple sensors which can detect the marks on the ceiling. Colleagues could simply key in the destination on its display panel, ‘DeliverBot’ will then automatically navigate to the designated location. It will return to the charging station and go into standby mode after completing its tasks and being disinfected by healthcare workers. It offers a helping hand in the ward and colleagues plan to extend the application of robot to frontline operation.

Healing at a distance
Delivery of healthcare services goes on during the outbreak of COVID-19, rain or shine. Tele-care plays a vital role in resuscitation of critical patients between Accident and Emergency Department of Tin Shui Wai Hospital and Intensive Care Unit (ICU) of Pok Oi Hospital (POH). This eICU initiative consists of various sophisticated sensors and Internet of Medical Things. By using high resolution cameras, Bluetooth stethoscope and data transmission software, doctors from the two hospitals can conduct clinical assessment, view ultrasound images and monitor patient’s vital signs in real time, thus more accurately determine whether the patient should be transferred to POH or Tuen Mun Hospital for further intensive care. It not only offers timely consultation, but also saves the time of patient transfer.

The 5G era in operating theatres
The demand for tele-care services has increased during the pandemic. Tseung Kwan O Hospital is the first to build a 5G network in the hospital which covers its operating theatres (OT). When surgeons need to consult with other medical professionals during an operation, they can instantly share the endoscopic images through the 5G smart glasses they are wearing via the 5G network. With 5G technologies, data and images can be transmitted at ultrahigh speed, allowing the situation in the OT to be viewed by senior doctors outside through mobile devices such as mobile phones and tablets. By examining the 3D images of the surgery, the senior doctors can grasp the details of the operation and patient’s situation in real time, and provide guidance remotely to improve the efficiency and accuracy of the operation.
Furthermore, Kowloon East Cluster has first implemented a tele-care pilot programme since the beginning of the pandemic. Patients at home are provided with tele-care examination and consultation, in order to reduce the risk of infection of healthcare workers and patients. The team is also exploring the use of vital sign monitoring equipment. Patients will be guided to use the equipment, so that data such as blood pressure, pulse and blood oxygen level will be transmitted to hospital instantly for medical staff’s monitoring.
Furthermore, Kowloon East Cluster has first implemented a tele-care pilot programme since the beginning of the pandemic. Patients at home are provided with tele-care examination and consultation, in order to reduce the risk of infection of healthcare workers and patients. The team is also exploring the use of vital sign monitoring equipment. Patients will be guided to use the equipment, so that data such as blood pressure, pulse and blood oxygen level will be transmitted to hospital instantly for medical staff’s monitoring.

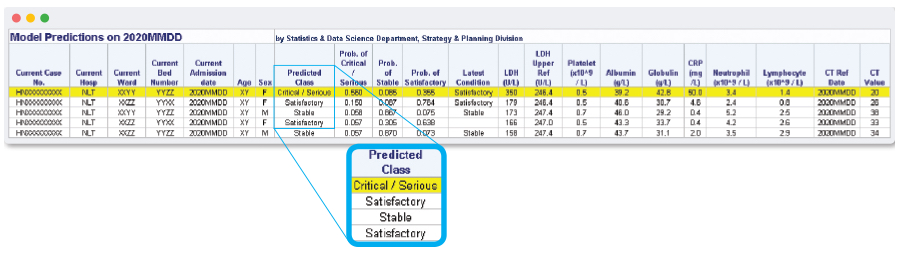
Big data analytics model supports triage at AWE
The Community Treatment Facility (CTF) at AsiaWorld-Expo (AWE) commenced operation in August for treating more stable COVID-19 patients to vacate isolation beds in hospitals for patients in more severe condition. The triage decision is based on the clinical judgment of doctors, but a big data analytics model has also served as an important reference prognostic tool in the process. This March, the Statistics and Data Science Department of the Head Office started to collaborate with clinical experts in developing a model to predict disease progression of patients through analytics of 30 patient data items. The team further simplified the model to using seven parameters, which include age, lab results of lactate dehydrogenase, C-reactive protein, platelet, neutrophil to lymphocyte ratio, albumin to globulin ratio, and assessed clinical condition. Based on individual patients’ latest blood test results and clinical condition, the model classifies patients into three outcome groups – ‘Critical / Serious’, ‘Stable’ and ‘Satisfactory’, and achieves a predictive accuracy rate of over 90%.
This prognostic tool has been applied to the daily operation of the CTF at AWE. Every morning at 7:00, a patient listing report is automatically sent to the relevant medical team for reference. After clinical assessment on patients’ conditions, potential deterioration cases are transferred to acute hospitals for treatment. Looking ahead, the team hopes to include additional model parameters, such as chest X-ray images, to assist doctors in monitoring patient disease progression.
This prognostic tool has been applied to the daily operation of the CTF at AWE. Every morning at 7:00, a patient listing report is automatically sent to the relevant medical team for reference. After clinical assessment on patients’ conditions, potential deterioration cases are transferred to acute hospitals for treatment. Looking ahead, the team hopes to include additional model parameters, such as chest X-ray images, to assist doctors in monitoring patient disease progression.
Video call for pharmaceutical care
The Telepharmacy Pilot Scheme, launched by the Pharmacy at Queen Mary Hospital since 2018, is targeted at all patients aged 18 or above, who have been discharged from or arranged for consultations at the hospital. Before meeting the pharmacist, the patient should be settled at home or in a quiet setting and prepare the medicine he is currently taking. During the video call, the pharmacist would assess patient’s symptoms, follow up on the use of medicines and therapeutic outcome, arrange medicine consultation and answer drug-related questions. Patients may arrange an appointment with pharmacists for enquiries from Mondays to Fridays. Pharmacists may also make proper arrangements subject to patients’ conditions.
