Clinical Services
Medicine

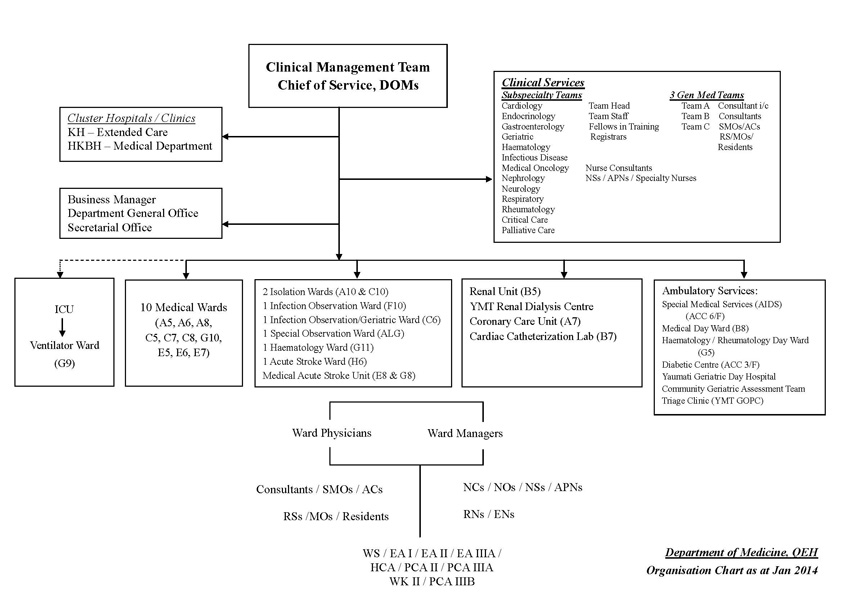
The Department of Medicine delivers high-quality multi-disciplinary care to patients with medical problems through a comprehensive range of secondary and tertiary subspecialty services, including Cardiology, Endocrinology, Gastroenterology & Hepatology, Haematology, Geriatrics, Infectious Disease, Medical Oncology, Nephrology, Neurology, Respiratory Medicine, Rheumatology and Palliative Care.
Our Renal Division is the pioneer center in Hong Kong providing Nocturnal Home Haemodialysis Programme to patients with end stage renal disease. We also operate one of the largest and most successful organ procurement and kidney transplantation program in the territory. In collaboration with other departments, our Neurology Division was amongst the first which provides 24-hour acute stroke thrombolysis service in the Hospital Authority. We have a fully accredited Endocrinology training center for the comprehensive assessment and management of patients with various endocrine disorders. A community diabetes complication screening programme helps to monitor disease control and provides early identification of complications. Our Cardiology Division provides a wide range of non-invasive and invasive cardiac diagnostic and therapeutic procedures. It has been the highest service volume cardiac center amongst all hospitals in Hong Kong for the decade. Our Gastroenterology & Hepatology Division offers a comprehensive range of diagnostic and therapeutic endoscopic procedures. Our Infectious Disease Division has successfully implemented Antibiotic Stewardship Programme and Outpatient Antibiotic Therapy programmes. Apart from providing a comprehensive Interventional Pulmonology service and being the pioneer in the introduction of flexi-rigid pleuroscopy in Hong Kong, our Respiratory Division has also collaborated with other divisions and departments in providing multi-disciplinary Sleep Disorder Breathing and Home Mechanical Ventilation Services. The work of the Department and its commitment to quality care is regularly awarded Outstanding Staff and Outstanding Team accolades by Queen Elizabeth Hospital and Hospital Authority.
Missions
- Quality patient care through teamwork
- Promoting specialty development while maintaining general medical service
- Enhance spirit of teamwork and collaboration among our staff and with other departments
- Emphasize training and career development for medical and nursing staff
- Develop service in line with the Hospital Authority direction and community expectation
- Conscientious of cost efficiency of clinical service
Vision
- To pursue excellence in clinical services
Value
- Respect
- Empathy
- Sharing
- Professionalism
- Efficiency
- Creativity
- Trust
Scope of Services
The inpatient service includes general and specialty wards, isolation and infection observation wards and other specialty ward facilities include as a coronary care unit, a haematology ward, two dialysis centers, a stroke ward as well as daywards covering cardiology, renal, haematology, rheumatology and general medical services to adult patients. Designated invasive mechanical and non-invasive ventilation areas are available in respiratory ward. The Department also provides joint professional services to patients at the special observation ward and the ventilator ward. It manages up to 59,000 in-patient episodes annually with over 50% being emergency admissions. Our comprehensive ambulatory care service includes specialist clinics and day wards which deal with 200,000 patients each year. We also operate a community geriatrics programme consisting of an out-reach team to elderly homes, pre- and post-discharge service, as well as a geriatric day hospital with around 10,000 attendances per year.
A. Acute Medical Beds
- Provide 24-hour quality medical and nursing care for medical patients admitted from the Accident and Emergency Department
- Manage common medical problems like coronary heart disease, stroke, diabetes, chronic bronchitis, and kidney failure etc., as well as many other rarer medical conditions
- Depending on the clinical progress and the expected length of stay, patients may be transferred to other medical wards, Extended Care Beds (in the Kowloon Hospital and the Buddhist Hospital) or other departments for continuation of care
B. Subspecialty Beds
- Provide comprehensive subspecialty in-patient services, including Cardiology, Endocrinology, Gastroenterology and Hepatology, Geriatrics, Haematology and Medical Oncology, AIDS Clinical Service, Infectious Diseases, Nephrology, Neurology, Respiratory Medicine and Rheumatology.
C. Coronary Care Unit (CCU)
- Intensive care centre for patients with acute heart conditions like acute myocardial infarction, severe unstable angina, acute aortic dissection and severe heart failure
- The Unit also provides early care for the post heart surgery patients, with joint consultations by our cardiologists and cardiothoracic surgeons
D. Isolation Beds
- Well-equipped isolation facilities for patients with potential infectious diseases, like influenza, pulmonary tuberculosis, infection with multi-drug resistant organisms, disseminated herpes zoster and chickenpox etc.
- Patients will be transferred out of the Isolation Beds when their infectious potentials have been excluded or controlled
- No visitors are allowed
E. Ventilator Beds
- Dedicated to specific patients with cardiopulmonary arrest or acute respiratory failure who require invasive or non-invasive mechanical ventilation support
F. Private Beds
- Both first-class and second-class beds are offered
G. Special Observation Beds
- Dedicated to management of mentally unstable patients
- Close liaison is maintained with the psychiatrists in the Kowloon Hospital
A. Medical Day Ward Services
Office Hour: Monday – Friday, 8am – 6pm
Closed during weekend and in public holidays
1. General
Introduction
- The general medical day ward is located on 8th floor, block B, main building of Queen Elizabeth Hospital.
- It serves medical patients with stable clinical conditions and with independent capacity in travelling between home and hospital.
- It ensures continuity of care to patients discharged from medical wards and allows medical treatments to be conducted in out-patient setting.
- Patients need not stay overnight and will be discharged on the same day if their medical conditions are stable and safe after assessment.
Benefits of Attending Out-patient Day Ward Services
- It shortens unnecessary wait for test results and investigations appointments in hospital.
- Risk of contracting infections inside hospital can be significantly reduced.
- Anxiety and depression associated with prolonged hospitalization can be minimized.
- Relatives can accompany patients to attend follow-up and to receive medical treatments.
They can have more time to discuss with the in-charge doctors on the medical conditions and progresses of the illnesses.
2. Cardiac
Introduction
With the aging population and the westernization of diet, patients having heart diseases are on growing trend. In line with the direction of HA clinical services, ambulatory service have to be strengthened. In 1995, QEH cardiac team has pioneered to establish Cardiac Day Centre. The objectives are to provide quality cardiac services to patients and at the same time to shorten length of hospital stay. In the beginning, activities were limited and focused on pre-operative preparation. With gradual expansion of services from year 2000 onwards, the number and variety of cardiac procedures and services have increased tremendously in Cardiac Day Centre. We have been awarded one of the Outstanding Teams of HA in 2008. The nurse clinic is the first Cardiology Nurse Clinic being accredited in HA in 2012.
In addition, QEH is the first hospital to start TAVI in HK and Greater China in 2010. Cardiac Day Centre serves as the coordination center for all the pre-TAVI assessment and post-TAVI follow-up echocardiogram arrangement.
3. Hematology
Hematology Day Ward Service
- Office hours: 09:00-17:00 Monday to Friday (except public holidays)
- Location: 5/F, Block G, Main Building
- Operated by Haematology doctors and nurses
- To provide ambulatory haematology service :
- Blood product transfusion
- Bone marrow aspiration and trephine biopsy
- Chemotherapy administration
- Hickman / Hemostar catheter care
- Plasmapheresis
- Leucopheresis
- Peripheral stem cell harvest
- Patient counseling
- Palliative care and support
4. Endocrine
Services
- Endocrine investigation
- Saline infusion test
- Short synacthen test (Low dose & standard dose)
- Insulin tolerance test
- Corticotropin-releasing factor (CRF) test
- Preparation of sampling procedure such as adrenal venous sampling, arterial stimulation venous sampling, bilateral inferior petrosal sinus sampling
- Patient education for learning home blood glucose monitoring and insulin injection
- DM monitoring and treatment
5. Respiratory
Introduction
Provides respiratory follow-up services, offers respiratory investigations and attends respiratory patients at out-patient setting.
Scope of Services
- Respiratory day clinic
- Day bronchoscopy service
- Out-patient ultrasound thorax , pleural tapping and pleural biopsy service
- Out-patient fine needle aspiration service
- Respiratory and medical oncology palliative care
- Home ventilation service
- CPAP assessment and compliance clinic
6. Rheumatology
Introduction
- The Rheumatology day ward is located on Block G, 5th floor of main building of Queen Elizabeth Hospital
- It provides rheumatology intravenous administration and early follow up and reviews of unstable rheumatic patients at inpatient setting, but patients need not to stay overnight
- Anti-Tumour Necrosis Factor therapy (Anti-TNF) for refractory rheumatoid arthritis and ankylosing spondylitis
- Anti-B cell therapy Rituximab for refractory rheumatic conditions
- Immunoglobulin for refractory rheumatic conditions
- Cyclophosphamide infusion for severe systemic lupus erythematosus or vasculitis
- Prostaglandin infusion for severe digital ischaemia
- It provides rheumatology nurse counseling at outpatient setting
- It provides ultrasound session at outpatient setting
B. Medical Subspecialty Clinics
1. B5 Renal Dialysis Center
Introduction
B5 Renal Unit is located in the main building of Queen Elizabeth Hospital. It provides dialysis service and follow up for patients with acute renal failure and end stage renal disease. It is also one of the major kidney transplant centers in Hong Kong.
Address
5/F, Block B, Renal Unit, Queen Elizabeth Hospital, 30 Gascoigne Road, Kowloon.
Scope of Service
- Peritoneal Dialysis
- Continuous Ambulatory Peritoneal Dialysis (CAPD)
- Automatic Peritoneal Dialysis (APD)
- Intermittent Peritoneal Dialysis (IPD)
- Chronic Hemodialysis
- Center-based Hemodialysis
- Acute Hemodialysis
- Hemofiltration
- Plasmapharesis
- Renal Palliative Care Programme
- Education Class
- Pre-dialysis Class
- Transplant Talk
- Renal Rehabilitation Programme
2. T3 Renal Dialysis Center
Introduction
T3 Renal Dialysis Center is a satellite dialysis center located in the new ACC Extension Block (Block T) of Queen Elizabeth Hospital. It provides dialysis service and follow up for patients with end stage renal disease. The center is closely connected with the B5 Renal Unit of Queen Elizabeth Hospital, providing seamless renal service for the patients in Kowloon Central Cluster Region.
Scope of Service
- Kidney Transplantation
- Peritoneal Dialysis
- Continuous Ambulatory Peritoneal Dialysis (CAPD)
- Automatic Peritoneal Dialysis (APD)
- Chronic Hemodialysis
- Nocturnal Home Hemodialysis
- Pre-dialysis Education Class
- Renal Rehabilitation Programme
Address
3rd Floor, ACC Extension Block (Block T), Queen Elizabeth Hospital
Telephone Number
35064060
Fax Number
35064068
3. Geriatric Day Hospital
Introduction
Geriatric Day Hospital (GDH) provides multidisciplinary assessment and intervention for elderly patients in Kowloon Central Cluster Region. It serves elderly with stable clinical conditions and provides rehabilitation to patients discharged from acute or convalescent hospitals, and also receive referrals from out-patients clinics or community geriatric assessment service. Standard referral form and initial geriatrician assessment are needed. All patients will be discharged on the same day. Transportation is provided based on need and availability.
Roles
- Serves as a time-limited and transitional continuum of in-hospital care to support early patient discharge from HA hospitals.
- Provides integrated and multi-professional assessment and treatment
Scope of Service
- On a day setting with necessary hospital facilities and expertise support, it can provide a one-stop base to manage older patients with complex geriatric conditions that require integrated and coordinated inter-disciplinary assessment and treatment, in which, geriatricians, nurses, PT, OT, ST, podiatrist, MSW work together in services like: Post-discharge reconditioning, rehabilitation and management of conditions among elderly patients including stroke, neurocognitive disorders, fall and bone health, syncope, nutrition and swallowing problems, spasticity, incontinence, etc.
- Support early discharge from hospital
- Head Up Tilt Table test
Staff Structure
- Geriatrician
- Unit Manager
- Advanced Practice Nurse
- Registered Nurse
- Enrolled Nurse
- Physiotherapists
- Occupational therapists
- Podiatrists from Podiatry Department
- Speech therapists from Department of Speech Therapy
- Medical social worker from Social Welfare Department
Office Hour
Monday – Friday 8:45am – 5:33pm
Closed during weekend and on public holidays
Address
4/F, Block T, Queen Elizabeth Hospital,30 Gascoigne Road, Kowloon, Hong Kong
Telephone
3506 4107
4. ACC Clinic
C. Community Geriatric Assessment Service (CGAS) – QEH Team
Staff Structure
- Geriatricians
- Medical officers
- Advanced Practicing Nurses
- Registered nurses
Office Hour
Monday – Saturday 8:30am – 5:18pm
Closed on Sundays and public holidays
Scope of Service
- Follow-up and clinical assessment of patients at elderly homes
- Ad hoc visits for semi-urgent clinical problems to reduce avoidable emergency admission
- Management of outbreaks of infectious diseases
- Early Supported Discharge
- Pressure Ulcer Program
- Enhancement of CGAT Service for EOL Care in Residential Care Homes for Elderly
- Clinical admission for patients requiring in-patient management
- Case conference
A. Medical Subspecialties
1. Cardiology
Staff Structure
- Cardiologists and Fellow trainees
- Cardiac nurses and paramedical staff
Service Scope
- Two Cardiac Catheterization Laboratories
- 7th Floor, Block B, Main Building
- Operation time: Monday - Friday, 09:00-17:00
- On-call emergency service
- Services include:
- Coronary angiography and cardiac catheterization
- Percutaneous transluminal coronary angioplasty and stenting
- Intravascular ultra-sound
- Electrophysiological studies
- Radiofrequency catheter ablation
- Pacemaker, Cardiac resynchronization therapy, Implantable cardioverter defibrillator implantation
- Percutaneous transvenous mitral commissurotomy
- Percutaneous congenital and structural heart interventions e.g. LAAO, TAVI
- Intra-cardiac echocardiogram
- Percutaneous transvenous endocardial biopsy
- Cardiac Care Unit
- 7th Floor, Block A, Main Building
- 10 Coronary Care Beds: Acute In-patient Care, Rehabilitation Program
- 5 Cardiac Intensive Care Beds: Immediate Post Open Heart Surgical Care
- Echocardiography Laboratory
- 7th Floor, Block B, Main Building
- Operation time:(Monday-Friday, 09:00-17:00)
- Transthoracic and transesophageal echocardiograms
- Non-invasive Cardiac Procedures (at EDU)
- 1st Floor, Block F, Main Building
- Operation time :(Monday-Friday, 09:00-17:00)
- 24-hour ambulatory monitoring of ECG (Holter) and blood pressure, activated recorders, exercise electrocardiography, cardiopulmonary assessment
- Cardiac Ambulatory Care Centre (B8C)
- 8th Floor, Block B, Main Building
- Operation time:(Monday-Friday, 08:00-20:00)
- To provide care for pre cardiac intervention preparation
- To provide care to patients after cardiac intervention and facilitate same day discharge such as coronary angiogram, percutaneous intervention (PCI), pacemaker implantation and EPS
- Cardiac Rapid Response Team to liaise patients presenting with STEMI going primary PCI
- One stop service for ACS patient to streamline earlier management strategy including arrangement of earlier in-patient coronary interventions
- Cardiology Nurse Clinic with four sub-clinic: Anticoagulation, CHF , post PCI, ACS/AMI nurse clinic. Aim to provide quality care to patients
- Co-ordination centre for TAVI and LAAO program
- Support other departments such as pacemaker programming
- Research activities co-ordination
- Cardiac Specialty Beds in General Ward
- 7th Floor, Block C, Main Building - 8 male in-patient beds
- 8th Floor, Block A, Main Building -8 female in-patient beds
-
Cardiac Specialist Out-patient Clinic & Staff Clinic
3rd Floor, ACC building and L-block -
Pacemaker Clinic and Pregnancy Clinic
3rd Floor, ACC building -
Cardiac Rehabilitation Program
In collaboration with dietitians, physiotherapists, occupational therapists to provide a comprehensive cardiac rehabilitation program (phase I-IV)
2. Endocrinology
Staff Structure
- Endocrinologists / Diabetologists
- Nurse Consultant
- Nurse Specialists
- Advanced Practice Nurse
- Diabetes / Metabolic Nurses
Service Scope
- Clinics (Endocrine, Diabetes, Thyroid, Gestational)
- Endocrine Specialty beds
- Ward and clinic consultations
- Special investigation at Endocrine Day Ward
- Diabetes education classes and individual counseling sessions at Diabetes Centre
- Ambulatory insulin adjustment and phone consultations for patients at Diabetes Centre
- Annual Diabetic Complication Assessment at Diabetes Centre
- Patient education
3. Gastroenterology and Hepatology
Staff Structure
- Gastroenterologists
Service Scope
- Inpatient Services
- Specialty beds
- Acute gastrointestinal bleeding care beds
- Outpatient Clinics
- Specialist out-patient clinic
- Consultations
- Endoscopy
- Oesophagogastroduodenoscopy
- Colonoscopy
- Endoscopic retrograde cholangiopancreatography
- Enteroscopy
- Endoscopic ultrasound
- Capsule endoscopy
- Percutaneous endoscopic gastrostomy
- Sigmoidoscopy
- Special Investigations
- 24-hr pH study
- urea breath test
- manometry
- fibroscan
- Liver Biopsy
- Ultrasound of hepatobiliary system
4. Geriatrics
Staff Structure
- Geriatricians
- Advanced Practicing Nurses
- Registered Nurses
Service Scope
- Inpatient Services
- Inpatient management of elderly patients
- Intra- and inter-departmental geriatric consultations
- Geriatric subspecialty beds
- Geriatric rehabilitation / convalescent bed in Hong Kong Buddhist Hospital
- Outpatient Clinics
- Geriatrics Specialty Clinics
- Memory Clinic
- Dizziness / Syncope Clinic
- Outpatient Services
- Cluster-based Integrated Care and Discharge Support Service (ICDS) ( Previously known as Integrated Care Model – ICM)
- Cluster Service Response Team
- Community Geriatric Assessment Service (CGAS)
- Geriatric Day Hospital (GDH)
- Collaborative Services
- Geriatric Pain Assessment Clinic - in collaboration with Pain Team of Department of Anesthesia
- Pre-Discharge service - in collaboration with QEH Pre-discharge team
- Instrumental Swallowing Assessment Service - in collaboration with Speech Therapist
5. Hematology and Oncology
Staff Structure
- Haematologists
- Haematology Nurse Specialists and Haematology Nurses
Service Scope
- In-patient Service
- Designated Haematology beds in Department of Medicine
- Haematology in-patients are under direct care from a team of clinical haematology staffs
- Out-patient Service
- 4 Haematology clinic sessions each week
- Haematology Day Ward Service
- Office hours: 09:00-17:00 Monday to Friday (except public holidays)
- Operated by Haematology doctors and nurses
- To provide ambulatory haematology service :
- Blood product transfusion
- Bone marrow aspiration and trephine biopsy
- Chemotherapy administration
- Hickman / Hemostar catheter care
- Plasmapheresis
- Leucopheresis
- Peripheral stem cell harvest
- Patient counseling
- Palliative care and support
6. AIDS Clinical Service
Scope of Service
AIDS Clinical Service at Queen Elizabeth Hospital started since 1985. We provide a comprehensive and integrated treatment program including in-patient service, rehabilitation and ambulatory care to HIV-infected adults and children. We aim at providing holistic and quality care to our patients.
- In-patient Service
- Acute care for the management of opportunistic infections & malignancies
- Rehabilitation
- Palliative care
- Ambulatory Care
Out-patient clinics - Provide holistic care to PLHIV
- Counseling and psychosocial support to patients, their partners and families
- Drug adherence program
- Genotypic resistance testing
- Partner referral and testing
- NeuroAIDS consultation service
- Medical oncology consultation service for AIDS-related malignancies
- Sub-specialty clinics including dermatology, gastroenterology, respiratory, nephrology, and palliative care medicine
- Day care center
- Women's health program including regular Pap smear examination
- Partnership with NGOs to foster community care
- Accredited Nurse Clinics
- Accredited by Hospital Authority since 2009
- Conduct nursing case management program to assure coordinated patient care
- Clinical Psychology Service
- Provide psychological intervention to PLHIV and their significant others
- Provide neuropsychological assessment and services to patients
- Post-exposure Prophylaxis Clinic
- Referral center for occupational exposure after needle-stick injury or mucosal contact
- Provide counseling, risk assessment, and offer prophylaxis if necessary
Team
We have a multidisciplinary care team with HIV physicians, ID specialists, pediatricians, nurses, clinical psychologist, medical social worker, dietitian, occupational therapists, clerical and supporting staff.
Our service is also supported by various specialists (microbiologist, dermatologist, neurologist, pulmonologist, gastroenterologist, hematologist, medical oncologist, nephrologist and palliative care physician)
Contact Us
Telephone number: (852) 3506 5855
Fax number: (852) 2783 7415
Clinic address: T Block, Queen Elizabeth Hospital, 30 Gascoigne Road, Kowloon, Hong Kong SAR
7. Infectious Disease
Staff Structure
- 3 Specialists
Service Scope
- Provide intra- and inter-departmental consultations in both inpatients and outpatients
- Provide inpatient care to patients with infectious diseases and/or HIV/AIDS
- Conduct weekly Infectious Diseases service round with microbiologists, paediatricians, pharmacists and infection control nurses
- Provide clinical services to patients with HIV/AIDS in both inpatients and outpatients
- Promote appropriate use of antimicrobials in the Antibiotic Stewardship Program (ASP)
- Collaborate with Infection Control Team (ICT), microbiologists, and Centre for Health Protection (CHP) in the management of hospital infectious diseases emergencies and outbreaks
- Collaborate with ICT and microbiologists to develop written policies and guidelines for infection control
- Collaborate with Community Geriatric Assessment Team (CGAT) and CHP on the management of infectious diseases outbreaks in the aged homes
- Collaborate with different clinical specialties on the development of infectious diseases management guidelines
8. Nephrology
Staff Structure
- Nephrologists
- Nursing Consultant
- Renal Nurses
Service Scope
- Inpatient Services
- Designated Nephrology Subspecialty Beds in C5 (male) and A5 (female) Wards
- In-patient Nephrology Consultation
- Outpatient Clinics
- Specialist Clinic in Queen Elizabeth Hospital
- B5 Renal Unit in Queen Elizabeth Hospital
- T3 Renal Dialysis Center
- Services
- Kidney Transplantation
- Peritoneal Dialysis
- Continuous Ambulatory Peritoneal Dialysis (CAPD)
- Automated Peritoneal Dialysis (APD)
- Intermittent Peritoneal Dialysis (IPD)
- Chronic Hemodialysis (HD)
- Center-based Hemodialysis
- Nocturnal Home Hemodialysis (NHHD)
- Acute Hemodialysis
- Hemofiltration
- Plasmapharesis
- General Nephrology
- Renal Palliative Care Programme
- Renal Rehabilitation Programme
- Public Education
- Pre-dialysis Class
- Transplant Talk
- Research Activities
- Renal Biopsy
- Dialysis Access Creation
9. Neurology
Staff Structure
- Neurologists
- Stroke Specialty Nurses
- Technical Services Assistant
Service Scope
- Inpatient Services
- Inpatient management of neurology patients
- Intra- and inter-departmental neurology consultations
- Acute Stroke Unit (ASU): A total of 30 stroke beds
- Combined Neurology and Neurosurgical wards
- Outpatient Clinics
- Neurology Specialty Clinics
- Combined Neurology-Oncology Clinic (in Department of Clinical Oncology)
- Botulinum Toxin Injection Clinics for Movement Disorders (in QEH) and Voice Disorders (in Yau Ma Tei ENT Specialist Clinic Extension)
- Integrated Deep Brain Stimulation Surgery Clinic for Movement Disorders
- Integrated Epilepsy Surgery Clinic
- Multiple Sclerosis Clinics
- Home Mechanical Ventilator Clinic (in B8 Dayward)
- Community Stroke Program Clinic (in Central Kowloon Health Centre)
- Tertiary Services
(in Collaboration with Intensive Care Unit and Departments of Accident and Emergency, Neurosurgery, Surgery, and Radiology and Imaging) - 24-Hour intravenous thrombolytic therapy for acute ischemic stroke
- Combined Carotid Intervention Services
- Epilepsy surgery
- Deep brain stimulation surgery
- Neurophysiology Study Services
- Interpretation and reporting of all adult electroencephalograms in QEH
- Nerve conduction and electromyography study sessions
- Long-term video-electroencephalographic monitoring
- Transcranial doppler studies
- Interpretation and reporting of all adult evoked potential studies in QEH (except intra-operative monitoring)
- Intra-operative neurophysiology monitoring of carotid endarterectomy and deep brain stimulation
- Neuropsychology Services
- Assessment of cognitive function
- Pre-surgical evaluation of refractory epilepsy patients
- Pre- and post-surgical evaluations of advanced Parkinson's disease patients
10. Respiratory Medicine
Staff Structure
- Respiratory specialists
- Fellow-in-training
- Advanced practice nurses
- Specialty nurses
Staff Structure
- In-patient Service
- Respiratory sub-specialty cares and sub-specialty beds
- Respiratory consultation services
- Respiratory infections and Tuberculosis care
- Acute non-invasive ventilation care
- Palliative Care for patients with end-stage respiratory diseases and lung cancer
- Out-patient Service
- Asthma clinic
- Chronic obstructive pulmonary disease clinic
- General respiratory clinic
- Palliative Care Clinic for patients with end-stage respiratory diseases and lung cancer
- Sleep disordered breathing clinic
- Respiratory Day-ward
- Respiratory day clinic
- Respiratory Nurse Clinic
- CPAP assessment and compliance care
- O2 Therapy Assessment & Titration clinic
- COPD & Asthma Nurse Clinic
- Lung Cancer Management Nurse Clinic
- Chronic Respiratory Disease Empowerment Program
- Sleep Related Breathing Disorder Nurse Clinic
- Skin Prick Test Nurse Clinic
- FOB Preparation Nurse Clinic
- Day bronchoscopy and EBUS service
- Ultrasound-guided thoracic interventions
- Indwelling pleural catheter (IPC)
- Home ventilation clinic (in collaboration with neurology team)
- Respiratory and medical oncology palliative care
- Pulmonary Physiology Studies
- Pulmonary function tests
- Cardio-pulmonary exercise test
- Skin prick test
- Methacholine challenge test
- Sleep Disordered Breathing and Chronic Respiratory Failure
- Sleep study
- CPAP and BIPAP titration
- Home ventilation service for patients with neuromuscular disorders (in collaboration with neurology team)
- Home ventilation service for patients with other chronic respiratory failure e.g. COPD, Obesity hypoventilation, kyphoscoliosis etc
- Interventional Pulmonology Services
- White light bronchoscopy
- X-ray guided bronchoscopy
- Auto-fluorescent bronchoscopy
- Cryotherapy
- Argon plasma coagulation (APC)
- Medical thoracoscopy
- Endobronchial ultrasound (EBUS)
- Endobronchial valve (EBV)
- Electromagnetic navigation bronchoscopy (ENB)
11. Rheumatology
Team
- Rheumatologists
- Rheumatology specialty nurse
Service Scope
Covering inflammatory rheumatic diseases
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Ankylosing spondylitis
- Psoriatic arthropathy
- Systemic necrotising vasculitis
- Dermatomyositis
- Difficult gouty arthritis
- In-patient Services
- In-patient management of rheumatology patients
- Intra- and inter-departmental rheumatology consultations
- Rheumatology day ward with biologic infusion and case review
- Rheumatology on-call service
- Rheumatology Grand Round
- Outpatient Services
- Specialist clinic
- Combined clinic (rheumatologist, orthopaedic surgeon, occupational therapist and podiatrist)
- Consultation Clinic
- Tight control rheumatoid arthritis Clinic
- Rheumatoid arthritis nurse clinic
B. Nursing Subspecialties
1. Nursing Specialty Services
1.1 Respiratory Nurse Specialty Service
The respiratory specialist nurse service provides inpatient and outpatient support to patients suffering from chronic respiratory diseases such as Chronic Obstructive Pulmonary Disease, Asthma, Obstructive Sleep apnoea and lung cancer etc.
Nursing Workforce
- Advanced Practice Nurses
- Registered Nurses
Objectives
- Perform general and respiratory assessments
- Provision of advice and support to the patients in their treatment process
- Liaise with other departments & healthcare professionals to provide integrated and patient-centered comprehensive care.
- To refresh, prepare & improve nurses with Respiratory specialty knowledge & related respiratory care
- Continuous education in light of their progress and new medical advances to achieve patient empowerment
- Regular patient reviews between physician assessments. Inputs might be provided on adjustments or titrations of therapy. These would also enhance the continuity of care and enable a nursing-patient relationship to be developed.
- Provision of intensive management during an acute exacerbation of airway diseases with advice and support in such difficult periods.
Nurse Assessment & Education Clinic
- COPD nurse Clinic
- Asthma Nurse Clinic
- Sleep Related Breathing Disorder Clinic
- CPAP Compliance & Assessment Clinic
- FOB Preparation Nurse Clinic
- Lung Cancer Management Clinic
- Skin Prick Test Nurse Clinic
- Chronic Lung Disease Empowerment Programme Clinic
- Oxygen Therapy Assessment Clinic
Staff Structure
- Provide education on basic concepts in the management of chronic respiratory diseases e.g. Asthma, COPD etc.
- Educate, assess and review the skills of using inhalers and spacers.
- Peak flow meter monitoring and self management plan in indicated asthma patients
- Smoking cessation counseling
- Home management of COPD, with a view for the possible necessity of home O2, home nebulizers, referrals for pulmonary rehab, etc.
- Allergen avoidance and management in difficult asthmatics
- Education to individual patients with diagnosed sleep apnea
- Monitoring of compliance to the treatment of chronic lung diseases and sleep apnea syndrome.
- Telephone advice & Follow-up service
- BIPAP (Bi-level Positive Airway Pressure) titration & education for patients undergoing arrangement for home mechanical ventilation
- Coordination of Home NIV (Non-Invasive Ventilation) programme in respiratory ward
- Periodically assess, review & advice on the care of NIV (Non-Invasive Ventilation) patients in medical wards
- Provide timely arrangement of CPAP titration for indicated in-patients with complicated cases documented or suspected OSA.
- Overnight oximetry monitoring for management of patients with chronic lung diseases in titration of oxygen or non-invasive ventilation therapies
- Perform bedside Lung Function Spirometry and TCO2 monitoring
- Assess and monitor patients on oxygen therapy at more precise regime identification and to prevent unnecessary O2 consumption for respiratory patients on short burst or long term oxygen therapy
- Arrange or assist in arranging investigations for the workup of patients with lung cancer. Monitor the progress of the patients and coordinating investigation results for multi-disciplinary team (MDT) case conference
- Facilitate and coordinate the continuity care of newly diagnosed lung cancer patients in order to provide access to appropriate services and acting as an information and education resource and support.
- Initiate and participate in evidenced-based practice & nursing research
- Develop professional nursing care protocols & regular respiratory audits
1.2 Special Medical Clinic
Special Medical Clinic provides comprehensive care to people infected and affected by HIV infection across the continuum of care.
Scope of Service
The nurses in Special Medical Service take up the role of case manager. The range of nursing services covers both in-patient and ambulatory care, it includes nursing assessment and counseling for newly diagnosed HIV patients and continuous counseling on subsequent follow-up visits, counseling and supporting of significant others, HIV screening for spouse and partners.
The Special Medical Clinic works closely with other disciplines; the nurses would make direct referrals to the multidisciplinary care team and leads the psychosocial round for in-patients.
We mobilize and locate community resources for individual patients while making discharge planning; and conduct regular case conference with AIDS-related non-government organization to ensure continuity of care.
Other services include therapeutic drug monitoring program to implement the strategies for successful adherence to antiretroviral therapy; deliver sexual health education and strategy of secondary prevention for individual patients; women health program with Pap smear screening and sexual health counseling for female patients of children age; pediatric care with family approach and empower patients via patient support group.
The team also provides post exposure prophylaxis counseling; risk assessment and support services to colleagues who sustained needle stick injury from source patients with HIV infection.
1.3 Rheumatology Nurse Specialty Service
The role of Rheumatology nurse is to enable and empower rheumatology patients to maintain and improve their physical, psychological and social functioning throughout their journey. Rheumatology nurse services are operates in a variety of settings including inpatients (hospitalized patients and day ward patients) and outpatients.
Scope of Services
Covering inflammatory rheumatic disease
- Rheumatoid arthritis
- Ankylosing spondylitis
- Psoriatic arthropathy
- Systemic lupus erythematosus
- Vasculitis
- Undifferentiated connective tissue disease
Specific Services
Rheumatology Nurse Clinic
-
Patient Education:
Assess individual needs and deliver medical education about the disease process and management of the disease. -
Counseling:
Assess patient's psychological needs and provide ongoing psychological support during the patient education process and telephone advice line. -
Drug Counseling and Monitoring:
Provide information regarding the benefits and potential side-effects of the medication according to guidelines for patients who are prescribed a new medication by the rheumatologist. Monitor the therapeutic effects and adverse effects of the prescribed drugs arise from the patients via phone follow up and review their blood test results. -
Coordinating Care:
Provide individual assessment of patients’ physical, psychological and social needs and referring them to other members of multidisciplinary team accordingly e.g. occupational therapy for splintage and assistive devices in daily living, podiatry for special footwear and foot caring, physiotherapy for exercise and pain relief and social welfare department for financial issue. -
Procedure:
Arrange and assist patients in receiving specific procedure e.g. joint tapping and intra-articular injection. -
Running a Telephone Advice-line:
Provide an access to patients and other health care professionals for advices on different aspects of care in rheumatology diseases. Monitor unstable patients’ condition via phone follow up. -
Drug Therapy:
Provide assessment, arrangement, administration and ongoing management of patients receiving biologics therapies and cytotoxic drugs e.g. infliximab and cyclophosphamide infusions. Provide intramuscular depot-steroid monthly as bridge therapy when necessary according to protocol. -
Wound Care:
Provide assessment and monitoring for difficult wounds e.g. vasculitic lesion/ulcer and referring to other specialty accordingly e.g. orthopedic nurse specialist. -
Educational Tool:
Develop professional nursing care protocols
1.4 Diabetes & Metabolic Centre
Workforce
- Nurse Consultant
- Nurse Specialist
- Advanced Practice Nurse (APN)
- Registered Nurse (RN)
Scope of Services
-
The Endocrinology Nurse Clinic (Diabetes)
QEH Endocrinology Nurse Clinic (Diabetes) is serviced by Diabetes Specialty Nurses and was first accredited as a Nurse Clinic by Hospital Authority in 2008.
Objectives- To assist diabetic patients and their immediate others in applying knowledge and skills learned into day-to-day diabetes self-care management.
- To empower diabetic patients with knowledge and skills in order to make informed choices concerning their diabetic management, and to support them emotionally.
- To facilitate behavioral changes in diabetic patients and promote a healthy life-style through education, so that the quality of life for diabetic patients are improved.
- To initiate preventive measures by performing comprehensive diabetic complications screening for diabetic patients and provide appropriate treatments and education.
- To ensure nursing care standard is followed so that the quality of care for diabetic patients is maintained.
- To assist in the formation of patient support group and provide professional support.
- To provide family planning advice to childbearing aged women with diabetes.
- Health assessment / Interpretation of investigation results
- DM education – providing DM knowledge, advising lifestyle modification, teaching DM self monitoring technique
- DM control / stabilization / Drug dosage adjustment / Telephone consultation
- Care planning / Prevention of complications
- Compliance empowerment / Counseling
- Evaluation of outcomes
- Referral to other disciplines as indicated e.g. dietitian, podiatrist, ophthalmologist, endocrinologist, diabetes patient support group, drug compliance clinic.
Diabetes Patient Empowerment Session – Diabetes ACC College Program
Teaching patient self-insulin injection
-
The Endocrinology Service
Objectives
- To well prepare patient both physically and psychologically for special investigations
- To conduct investigations for patient safely and correctly
- To provide patient education for better self-care
Services
Endocrine Investigations include:
- Saline infusion test
- Short synacthen test (Low dose & standard dose)
- Insulin tolerance test
- Corticotropin-releasing factor (CRF) test
- Sampling procedure such as adrenal venous sampling, arterial stimulation venous sampling, bilateral inferior petrosal sinus sampling
- Others: Staff Training, Research, Community Program, Patient Support Group
Contact Us
Address: Diabetes Centre, 9/F, T Block, Queen Elizabeth Hospital
Telephone: 3506 6574
Fax: 3506 6886
1.5 Acute Stroke Unit
The Acute Stroke Unit, established in 1996, is a 30-bed unit located on one medical ward and two neuro-surgical wards. The unit provides specialized care to patients who have suffered a stroke or transient ischemic attack. The unit utilizes a team approach to patient care including the neurologist, nurse, physiotherapist, occupational therapist, dietitian and speech therapist. The RN is the primary care provider and works closely with other team members to provide quality patient care.
The 24 hrs intravenous thrombolysis programme for acute ischaemic stroke started from December, 2008. Intravenous recombinant tissue plasminogen activator (rtPA, alteplase) is the only drug approved for the treatment of acute ischemic stroke and it should be administered within 3 hours of stroke. Standard operation guidelines, protocols and pathways are established and followed by all professionals. The guidelines equip the clinical team with mechanisms for coordinated care and clearly articulate the roles and responsibilities of the interdisciplinary clinical team during the emergency and acute phases of stroke. The Stroke Advance Practice Nurse is on call 24 hrs a day and works collaboratively with other clinical and medical professionals to provide comprehensive care.
The Stroke Nursing Officer focuses on patient and family education and assists the patients and their families in their efforts toward recovery and rehabilitation. He also provides specialty clinical supervision to the ward nurses and monitoring the progress of the stroke patient according to the critical pathway.
1.6 Renal Nurse Specialty Service
The nursing team in renal specialty provides a variety of care services to the in-patients and out-patients of the QEH renal unit and Yau Ma Tei Dialysis center. We have a team of over 40 dedicated renal nurses who offer the highest standard of care and support to all their patients. In regards to the diversity of renal services that include in-center hemodialysis, home hemodialysis; peritoneal dialysis, renal palliative care and kidney transplantation, we have integrated the nursing assessment, patient education and nursing interventions into systemic, with guidelines driven care management for patients receiving different types of treatment for their kidney disease.
Objectives
- Enhance a safe and high quality care services for patients receiving different mode of renal replacement therapies and renal palliative care.
- Empower the patients to live with dialysis in a full, active and healthy life.
- Reduce and prevent the dialysis complications to enhance a superb treatment outcome.
- Empower the patients with chronic kidney disease in delaying the progress of reaching End Stage Renal Disease.
- Provide a seamless patient centered care delivery system with multi-disciplinary teams support.
Scope of Services
- In-patient Services
- Provide renal nursing services for patients requiring acute and chronic hemodialysis, kidney transplant and hospitalized peritoneal dialysis patients.
- Provide home dialysis training programs including Continuous Ambulatory Peritoneal Dialysis (CAPD); Automated Peritoneal Dialysis (APD) and Nocturnal Home Hemodialysis (NHHD).
- We accept renal nursing consultation from the general wards of medicine for patients with kidney problems.
- Out-patient Services
- Patient education and counseling
- Organize pre-dialysis educational seminar 3 times per year.
- Organize pre-transplantation educational seminar 3 times per year
- Organize patient and family gathering for sharing of life adjustment changes with dialysis therapy 3 times per year.
- Renal Nurse Clinic
- Patients with chronic kidney disease:
- Provide primary health education for preservation of residue renal function.
- Arrange pre-dialysis physical psycho-social assessment.
- Provide clear patient information on peritoneal dialysis therapy which is the first treatment policy in Hong Kong; other treatments include hemodialysis, living related kidney transplantation or palliative care.
- Organize preparatory works for creation of vascular access and dialysis access.
- Patients on chronic dialysis therapy or kidney transplantation:
- Provide continuous monitoring, education or skill retraining for home dialysis therapy.
- Provide education, assessment and management of vascular access and peritoneal dialysis access.
- Arrange post kidney transplantation self-care education.
- Patients opted for renal palliative care:
- Provide symptoms management, nutritional assessment and dietary education.
- Offer supporting system via phone consultation.
- Collaborate with multi-disciplinary services to facilitate spiritual and social support for the patients.
- Patient Rehabilitation
- Give advices and support the activities organized by QEH renal patient support group.
- Collaborate with the physiotherapy department of QEH for the rehabilitation program of the dialysis patients.
- Active participation in the Hong Kong Transplant and dialysis games.
- Health Promotion
- Participate in World kidney day, Hong Kong Health Carnival.
- Support health promotional events organized by Hong Kong Association of Renal Nurses (HKARN) and Hong Kong Society of Nephrology (HKSN).
1.7 Cardiac Nurse Specialty Service
Objectives of Cardiology Nurse Clinic
- To empower patients and carers to participate in the process of maintaining/ improving their own health
- To integrate patient care from acute to community care
- To expand the role of nursing practice as case manager
- To prevent avoidable admission for relatively stable patient groups shorten their length of stay
- Better use of acute hospital beds in KCC
Scope of Services
- Anti-coagulation Nurse Clinic
- Comprehensive assessment / education on dietary, lifestyle and drug interaction
- Titrate dose of anticoagulant according to protocol tailor-made for Chinese patients
- Optimize coagulation profile to reduce length of hospital stay for warfarin overdose patients or unnecessary admission for suboptimal clotting profile
- To reduce the time of waiting for lab. result, patients will be informed and followed up by telephone
- Congestive Heart Failure (CHF) Nurse Clinic
- To promote / improve health seeking self-help behavior
- To maximize quality of life and symptoms monitoring
- Medication titration according to pre-set protocol
- Telephone hotline support during office hours
- Collaborate with NGO / patient self-help group for continuation of care
- Post Percutaneous Coronary Intervention (PCI) Nurse Clinic
- To provide nurse consultation at 1-2 weeks/ 6 months +/- PRN after PCI
- To monitor drug compliance
- To review and maximize medication according to set protocol
- Early detection of re-stenosis and possible complications
1.8 Gastroenterology and Hepatology Nurse Specialty Service
Objectives
- to promote the awareness and educate patient and family members about gastro-intestinal and liver disorders
- to provide nursing assessment and supporting services for the on-treatment patient
- to monitor on-treatment patient’s blood result and progress, to detect any adverse drug effect and alter treatment according to protocol and guidelines
- to conduct health education and empower patient to prevent drug resistance
Scope of Service
- to provide service and consultation to both in-patients and out-patients
- to provide education and counseling on gastro-intestinal and liver disorders
- to teach on-treatment patient injection skill and monitor patient’s performance
- to follow up patient during and after treatment
- to perform Fibroscan for in-patient and out-patient
Address
Department of Medicine
Queen Elizabeth Hospital
30, Gascoigne Road
Kowloon
Hong Kong
General Enquiries
35068888